Articles
- Page Path
- HOME > Acute Crit Care > Volume 39(1); 2024 > Article
-
Original Article
Pulmonary Association between mechanical power and intensive care unit mortality in Korean patients under pressure-controlled ventilation -
Jae Kyeom Sim1
 , Sang-Min Lee2
, Sang-Min Lee2 , Hyung Koo Kang3
, Hyung Koo Kang3 , Kyung Chan Kim4
, Kyung Chan Kim4 , Young Sam Kim5
, Young Sam Kim5 , Yun Seong Kim6
, Yun Seong Kim6 , Won-Yeon Lee7
, Won-Yeon Lee7 , Sunghoon Park8
, Sunghoon Park8 , So Young Park9
, So Young Park9 , Ju-Hee Park10
, Ju-Hee Park10 , Yun Su Sim11
, Yun Su Sim11 , Kwangha Lee12
, Kwangha Lee12 , Yeon Joo Lee13
, Yeon Joo Lee13 , Jin Hwa Lee14
, Jin Hwa Lee14 , Heung Bum Lee15
, Heung Bum Lee15 , Chae-Man Lim16
, Chae-Man Lim16 , Won-Il Choi17
, Won-Il Choi17 , Ji Young Hong18
, Ji Young Hong18 , Won Jun Song19, Gee Young Suh20
, Won Jun Song19, Gee Young Suh20
-
Acute and Critical Care 2024;39(1):91-99.
DOI: https://doi.org/10.4266/acc.2023.00871
Published online: January 26, 2024
1Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
3Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
4Department of Internal Medicine, Daegu Catholic University Medical Center, Daegu Catholic University School of Medicine, Daegu, Korea
5Division of Pulmonology, Department of Internal Medicine, Institute of Chest Disease, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
6Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
7Divison of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Yonsei University Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
8Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea
9Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Kangdong Sacred Heart Hospital, Seoul, Korea
10Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Dongguk University Ilsan Hospital, Goyang, Korea
11Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea
12Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea
13Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
14Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Ewha Womans University College of Medicine, Seoul, Korea
15Division of Respiratory Disease and Critical Care Medicine, Department of Internal Medicine, Jeonbuk National University Medical School and Hospital, Jeonju, Korea
16Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
17Department of Internal Medicine, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
18Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Chuncheon Sacred Heart Hospital, Hallym University Medical Center, Chuncheon, Korea
19Department of Critical Care Medicine, Sungkyunkwan University School of Medicine, Kangbuk Samsung Hospital, Seoul, Korea
20Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- Corresponding author: Gee Young Suh Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul 06351, Korea Tel: +82-2-3410-3429 Fax: +82-2-3410-6956 E-mail: smccritcare@gmail.com
© 2024 The Korean Society of Critical Care Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 677 Views
- 56 Download
Abstract
-
Background
- Mechanical power (MP) has been reported to be associated with clinical outcomes. Because the original MP equation is derived from paralyzed patients under volume-controlled ventilation, its application in practice could be limited in patients receiving pressure-controlled ventilation (PCV). Recently, a simplified equation for patients under PCV was developed. We investigated the association between MP and intensive care unit (ICU) mortality.
-
Methods
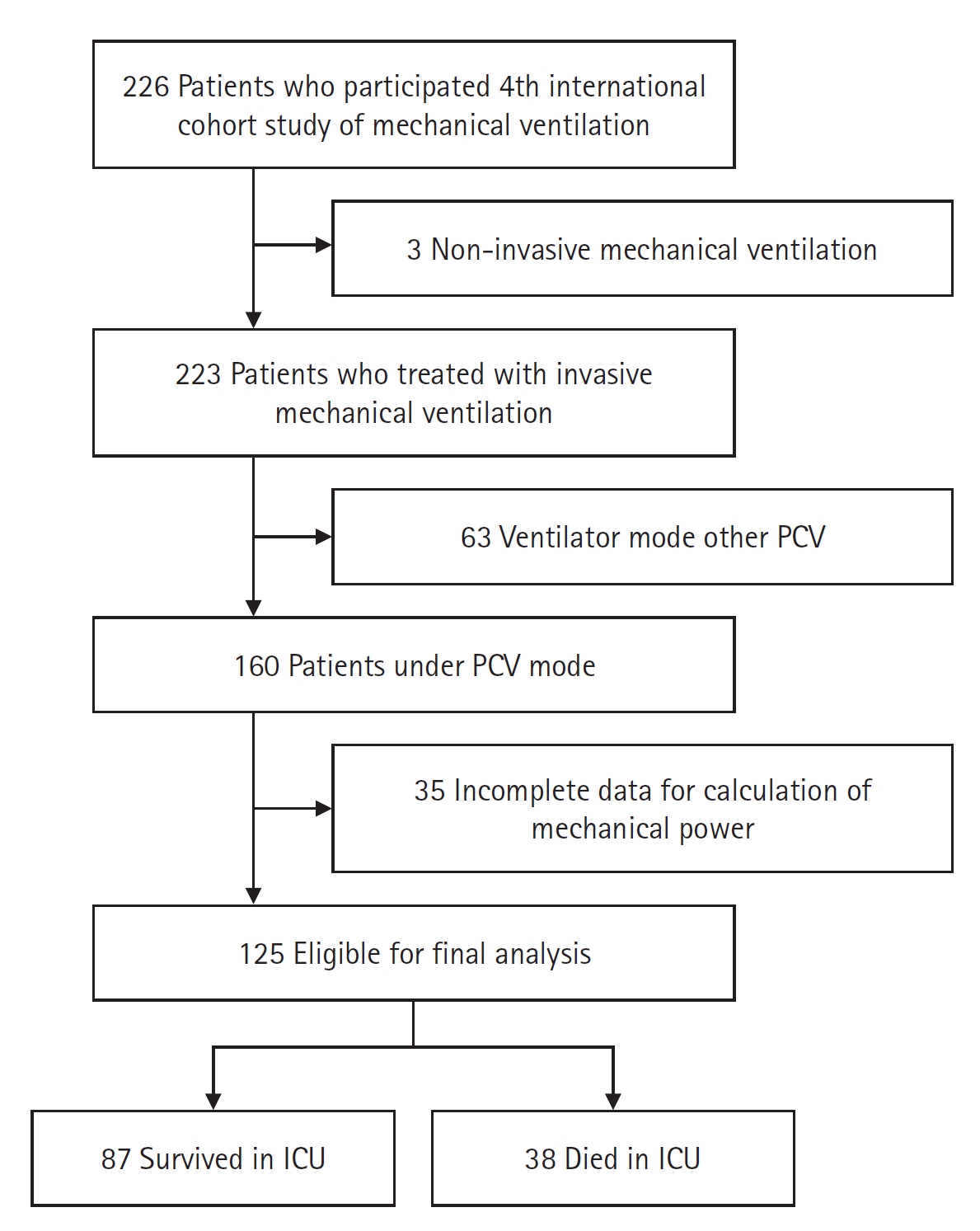
- We conducted a retrospective analysis of Korean data from the Fourth International Study of Mechanical Ventilation. We extracted data of patients under PCV on day 1 and calculated MP using the following simplified equation: MPPCV = 0.098 ∙ respiratory rate ∙ tidal volume ∙ (ΔPinsp + positive end-expiratory pressure), where ΔPinsp is the change in airway pressure during inspiration. Patients were divided into survivors and non-survivors and then compared. Multivariable logistic regression was performed to determine association between MPPCV and ICU mortality. The interaction of MPPCV and use of neuromuscular blocking agent (NMBA) was also analyzed.
-
Results
- A total of 125 patients was eligible for final analysis, of whom 38 died in the ICU. MPPCV was higher in non-survivors (17.6 vs. 26.3 J/min, P<0.001). In logistic regression analysis, only MPPCV was significantly associated with ICU mortality (odds ratio, 1.090; 95% confidence interval, 1.029–1.155; P=0.003). There was no significant effect of the interaction between MPPCV and use of NMBA on ICU mortality (P=0.579).
-
Conclusions
- MPPCV is associated with ICU mortality in patients mechanically ventilated with PCV mode, regardless of NMBA use.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
DISCUSSION
KEY MESSAGES
-
CONFLICT OF INTEREST
Kwangha Lee is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflict of interest relevant to this article was reported.
-
FUNDING
None.
-
AUTHOR CONTRIBUTIONS
Conceptualization: JKS, GYS. Data curation: all authors. Formal analysis: JKS, GYS. Visualization: JKS. Supervision: GYS. Writing–original draft: JKS. Writing–review & editing: SML, HKK, KCK, YSK, YSK, WYL, SP, SYP, JHP, YSS, KL, YJL, JHL, HBL, CML, WIC, JYH, WJS, GYS. All authors read and agreed to the published version of the manuscript.
NOTES
Acknowledgments
SUPPLEMENTARY MATERIALS
Supplementary Table 1.
Supplementary Table 2.
Supplementary Table 3.
Supplementary Table 4.
| Variable | All (n=125) | Survivor (n=87) | Non-survivor (n=38) | P-value |
|---|---|---|---|---|
| Age (yr) | 68 (57–78) | 68 (58–78) | 66 (55–75) | 0.425 |
| Male | 83 (66.4) | 58 (66.7) | 25 (65.8) | 0.924 |
| Weight (kg) | 60.0 (50.0–68.0) | 60.0 (49.0–68.0) | 60.0 (53.0–68.5) | 0.531 |
| Height (cm) | 165.0 (158.0–170.0) | 164.0 (157.0–170.0) | 165.5 (159.8–170.0) | 0.503 |
| BMI (kg/m2) | 22.0 (19.0–24.0) | 22.0 (19.0–25.0) | 22.0 (20.0–24.0) | 0.851 |
| SAPS II | 50 (40–61) | 50 (42–63) | 48.5 (36–60) | 0.205 |
| Primary reason for mechanical ventilationa) | 0.435 | |||
| Acute on chronic respiratory failure | 8 (7.3) | 5 (6.7) | 3 (8.6) | |
| COPD | 4 (3.6) | 3 (4) | 1 (2.9) | |
| Asthma | 2 (1.8) | 2 (2.7) | 0 | |
| Other chronic respiratory disease | 2 (1.8) | 0 | 2 (5.7) | |
| Acute respiratory failure | 91 (82.7) | 60 (80) | 31 (88.6) | |
| ARDS | 6 (5.5) | 2 (2.7) | 4 (11.4) | |
| Postoperative | 0 | 0 | 0 | |
| Congestive heart failure | 11 (10.0) | 9 (12.0) | 2 (5.7) | |
| Aspiration | 14 (12.7) | 12 (16) | 2 (5.7) | |
| Pneumonia | 30 (27.3) | 16 (21.3) | 14 (40) | |
| Sepsis | 20 (18.2) | 12 (16) | 8 (22.9) | |
| Trauma | 1 (0.9) | 1 (1.3) | 0 | |
| Cardiac arrest | 5 (4.5) | 5 (6.7) | 0 | |
| Other acute respiratory failure | 4 (3.6) | 3 (4) | 1 (2.9) | |
| Coma | 9 (8.2) | 8 (10.7) | 1 (2.9) | |
| Neuromuscular disease | 2 (1.8) | 2 (2.7) | 0 | |
| pHb) | 7.36 (7.29–7.45) | 7.38 (7.29–7.46) | 7.34 (7.27–7.41) | 0.230 |
| PaCO2 (mm Hg)b) | 39.0 (31.0–46.0) | 38.0 (31.0–51.0) | 40.0 (31.0–43.3) | 0.642 |
| PaO2 (mm Hg)b) | 87.0 (68.5–116.5) | 85.0 (67.0–120.0) | 89.5 (77.8–114.5) | 0.239 |
| PaO2/FiO2 ratiob) | 157 (106–230) | 165 (114–256) | 137 (95–211) | 0.105 |
| Analgesicb) | 98 (78.4) | 63 (72.4) | 35 (92.1) | 0.014 |
| Sedativeb) | 86 (68.8) | 57 (65.5) | 29 (76.3) | 0.231 |
| NMBAb) | 19 (15.2) | 10 (11.5) | 9 (23.7) | 0.081 |
Values are presented as median (interquartile range) or number (%).
BMI: body mass index; SAPS: Simplified Acute Physiology Score; COPD: chronic obstructive pulmonary disease; ARDS: acute respiratory distress syndrome; PaCO2: partial pressure of carbon dioxide; PaO2: partial pressure of oxygen; FiO2: fraction of inspired oxygen; NMBA: neuromuscular blocking agent.
a) Data were not available in 12 patients among survivors and 3 patients among non-survivors;
b) Data were collected at 8 am on day 1.
| Variable | All (n=125) | Survivor (n=87) | Non-survivor (n=38) | P-value |
|---|---|---|---|---|
| Mechanical power (J/min) | 21.7 (14.3–26.6) | 17.6 (12.7–23.7) | 26.3 (20.7–33.9) | <0.001 |
| VT/PBW (ml/kg) | 7.2 (6.2–8.7) | 7.0 (6.0–8.1) | 8.2 (6.6–9.2) | 0.025 |
| PEEP (cm H2O)a) | 5.0 (5.0–8.0) | 5.0 (5.0–8.0) | 7.0 (5.0–8.0) | 0.176 |
| Variable |
Univariable analysis |
Multivariable analysis |
||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Age (yr) | 0.989 (0.963–1.016) | 0.423 | 0.992 (0.961–1.026) | 0.652 |
| Male | 0.962 (0.430–2.150) | 0.924 | 1.109 (0.441–2.789) | 0.826 |
| BMI (kg/m2) | 1.009 (0.915–1.113) | 0.850 | - | - |
| SAPS II | 0.985 (0.963–1.008) | 0.205 | - | - |
| Primary reason for mechanical ventilation, acute respiratory ailure | 1.937 (0.592–6.337) | 0.274 | - | - |
| pHa) | 0.127 (0.004–3.683) | 0.230 | ||
| PaCO2 (mm Hg)a) | 0.978 (0.948–1.009) | 0.158 | 0.975 (0.938–1.013) | 0.191 |
| PaO2 (mm Hg)a) | 1.003 (0.996–1.010) | 0.426 | - | - |
| PaO2/FiO2 ratioa) | 0.997 (0.993–1.001) | 0.129 | 1.000 (0.995–1.004) | 0.844 |
| Analgesica) | 4.444 (1.249–15.816) | 0.021 | 3.568 (0.834–15.256) | 0.086 |
| Sedativea) | 1.696 (0.711–4.043) | 0.233 | - | - |
| NMBAa) | 2.390 (0.882–6.474) | 0.087 | 1.935 (0.606–6.178) | 0.265 |
| Mechanical power (J/min)a) | 1.105 (1.053–1.159) | <0.001 | 1.090 (1.029–1.155) | 0.003 |
| VT/PBWa) | 1.239 (1.022–1.502) | 0.029 | 1.079 (0.835–1.395) | 0.561 |
| PEEP (cm H2O)a) | 1.086 (0.920–1.283) | 0.329 | - | - |
Variables with P-value less than 0.2 in univariable analysis and clinical variables with important meanings (age, sex) were included in the multivariable analysis.
OR: odds ratio; CI: confidence interval; BMI: body mass index; SAPS: Simplified Acute Physiology Score; PaCO2: partial pressure of carbon dioxide; PaO2: partial pressure of oxygen; FiO2: fraction of inspired oxygen; NMBA: neuromuscular blocking agent; VT/PBW: tidal volume per predicted body weight; PEEP: positive end-expiratory pressure.
a) Data were collected at 8 am on day 1.
| Variable | OR (95% CI) | P-value |
|---|---|---|
| Non-use of NMBA | 1.081 (1.017–1.149) | 0.013 |
| Use of NMBA | 1.125 (0.987–1.283) | 0.078 |
| Interaction of MPPCV and NMBA | - | 0.579 |
- 1. Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med 2013;369:2126-36.ArticlePubMed
- 2. Cho YJ, Moon JY, Shin ES, Kim JH, Jung H, Park SY, et al. Clinical practice guideline of acute respiratory distress syndrome. Korean J Crit Care Med 2016;31:76-100.ArticlePDF
- 3. Hotchkiss JR, Blanch L, Murias G, Adams AB, Olson DA, Wangensteen OD, et al. Effects of decreased respiratory frequency on ventilator-induced lung injury. Am J Respir Crit Care Med 2000;161(2 Pt 1):463-8.ArticlePubMed
- 4. Chiumello D, Carlesso E, Brioni M, Cressoni M. Airway driving pressure and lung stress in ARDS patients. Crit Care 2016;20:276. ArticlePubMedPMC
- 5. Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med 2016;42:1567-75.ArticlePubMedPDF
- 6. Cressoni M, Gotti M, Chiurazzi C, Massari D, Algieri I, Amini M, et al. Mechanical power and development of ventilator-induced lung injury. Anesthesiology 2016;124:1100-8.ArticlePubMedPDF
- 7. Vassalli F, Pasticci I, Romitti F, Duscio E, Aßmann DJ, Grünhagen H, et al. Does iso-mechanical power lead to iso-lung damage?: an experimental study in a porcine model. Anesthesiology 2020;132:1126-37.PubMed
- 8. Scharffenberg M, Wittenstein J, Ran X, Zhang Y, Braune A, Theilen R, et al. Mechanical power correlates with lung inflammation assessed by positron-emission tomography in experimental acute lung injury in pigs. Front Physiol 2021;12:717266. ArticlePubMedPMC
- 9. Serpa Neto A, Deliberato RO, Johnson AE, Bos LD, Amorim P, Pereira SM, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med 2018;44:1914-22.ArticlePubMedPDF
- 10. Esteban A, Frutos-Vivar F, Muriel A, Ferguson ND, Peñuelas O, Abraira V, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med 2013;188:220-30.ArticlePubMed
- 11. Oh Y, Kang Y, Lee K. Development of a prognostic scoring system in patients with pneumonia requiring ventilator care for more than 4 days: a single-center observational study. Acute Crit Care 2021;36:46-53.ArticlePubMedPMCPDF
- 12. Murray MJ, DeBlock H, Erstad B, Gray A, Jacobi J, Jordan C, et al. Clinical practice guidelines for sustained neuromuscular blockade in the adult critically ill patient. Crit Care Med 2016;44:2079-103.ArticlePubMed
- 13. Becher T, van der Staay M, Schädler D, Frerichs I, Weiler N. Calculation of mechanical power for pressure-controlled ventilation. Intensive Care Med 2019;45:1321-3.ArticlePubMedPDF
- 14. Sim JK, Lee SM, Kang HK, Kim KC, Kim YS, Kim YS, et al. Change in management and outcome of mechanical ventilation in Korea: a prospective observational study. Korean J Intern Med 2022;37:618-30.ArticlePubMedPMCPDF
- 15. Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, Stewart TE, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA 2002;287:345-55.ArticlePubMed
- 16. Chi Y, Zhang Q, Yuan S, Zhao Z, Long Y, He H. Twenty-four-hour mechanical power variation rate is associated with mortality among critically ill patients with acute respiratory failure: a retrospective cohort study. BMC Pulm Med 2021;21:331. ArticlePubMedPMCPDF
- 17. Urner M, Jüni P, Hansen B, Wettstein MS, Ferguson ND, Fan E. Time-varying intensity of mechanical ventilation and mortality in patients with acute respiratory failure: a registry-based, prospective cohort study. Lancet Respir Med 2020;8:905-13.ArticlePubMedPMC
- 18. Tonna JE, Peltan ID, Brown SM, Grissom CK, Presson AP, Herrick JS, et al. Positive end-expiratory pressure and respiratory rate modify the association of mechanical power and driving pressure with mortality among patients with acute respiratory distress syndrome. Crit Care Explor 2021;3:e0583.ArticlePubMedPMC
- 19. van Meenen DM, Serpa Neto A, Paulus F, Merkies C, Schouten LR, Bos LD, et al. The predictive validity for mortality of the driving pressure and the mechanical power of ventilation. Intensive Care Med Exp 2020;8(Suppl 1):60. PubMedPMC
- 20. Jeong BH, Suh GY, An JY, Park MS, Lee JH, Lee MG, et al. Clinical demographics and outcomes in mechanically ventilated patients in Korean intensive care units. J Korean Med Sci 2014;29:864-70.ArticlePubMedPMCPDF
- 21. Peñuelas O, Muriel A, Abraira V, Frutos-Vivar F, Mancebo J, Raymondos K, et al. Inter-country variability over time in the mortality of mechanically ventilated patients. Intensive Care Med 2020;46:444-53.ArticlePubMedPMCPDF
- 22. Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med 2017;195:438-42.ArticlePubMed
- 23. van der Meijden S, Molenaar M, Somhorst P, Schoe A. Calculating mechanical power for pressure-controlled ventilation. Intensive Care Med 2019;45:1495-7.ArticlePubMedPDF
- 24. Trinkle CA, Broaddus RN, Sturgill JL, Waters CM, Morris PE. Simple, accurate calculation of mechanical power in pressure controlled ventilation (PCV). Intensive Care Med Exp 2022;10:22. ArticlePubMedPMCPDF
References
Figure & Data
References
Citations


 KSCCM
KSCCM
 PubReader
PubReader ePub Link
ePub Link Cite
Cite


