Articles
- Page Path
- HOME > Acute Crit Care > Volume 36(3); 2021 > Article
-
Image in Critical Care
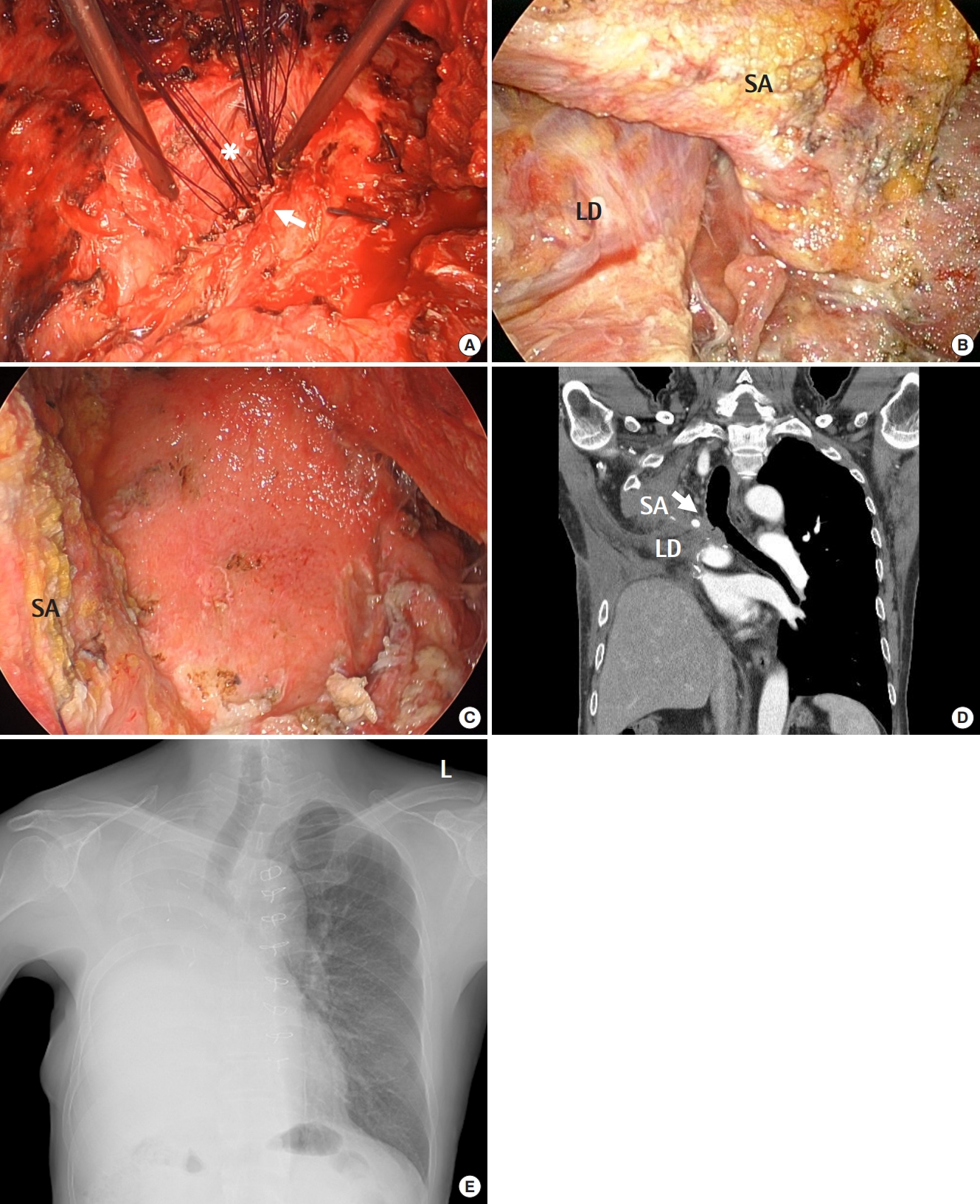
Thoracic Surgery Thoracomyoplasty and perioperative negative wound pressure therapy for bronchopleural fistula after trans-sternal bronchial closure -
Jinwook Hwang1,2
 , Jeong In Hong1
, Jeong In Hong1 , Hong Ju Shin1
, Hong Ju Shin1 , Jae Seung Shin1
, Jae Seung Shin1 , Je Hyeong Kim2,3
, Je Hyeong Kim2,3
-
Acute and Critical Care 2021;36(3):269-273.
DOI: https://doi.org/10.4266/acc.2021.00626
Published online: August 3, 2021
1Department of Thoracic and Cardiovascular Surgery, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
2Department of Critical Care Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
3Division of Pulmonology, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- Corresponding author Je Hyeong Kim Department of Critical Care Medicine, Korea University Ansan Hospital, Korea University College of Medicine and Division of Pulmonology, Department of Internal Medicine, Korea University Ansan Hospital, 123 Jeokgeum-ro, Danwon-gu, Ansan 15355, Korea Tel: +82-31-412-5950 Fax: +82-31-413-5950 E-mail: chepraxis@korea.ac.kr
Copyright © 2021 The Korean Society of Critical Care Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 3,063 Views
- 90 Download
-
CONFLICT OF INTEREST No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
Conceptualization: JH. Data curation: JIH. Formal analysis: JH. Methodology: JHK, Project administration: JSS, HJS. Visualization: JH. Writing–original draft: JIH, JH. Writing–review&editing: JH.
NOTES
- 1. Abruzzini P. Surgical treatment of fistulae of the main bronchus after pneumonectomy in tuberculosis (personal technic). Thoraxchirurgie 1963;10:259-64.PubMed
- 2. Fournier I, Krueger T, Wang Y, Meyer A, Ris HB, Gonzalez M. Tailored thoracomyoplasty as a valid treatment option for chronic postlobectomy empyema. Ann Thorac Surg 2012;94:387-93.ArticlePubMed
- 3. Botianu PV, Botianu AM. Thoracomyoplasty in the treatment of empyema: current indications, basic principles, and results. Pulm Med 2012;2012:418514. ArticlePubMedPMC
- 4. Hysi I, Rousse N, Claret A, Bellier J, Pinçon C, Wallet F, et al. Open window thoracostomy and thoracoplasty to manage 90 postpneumonectomy empyemas. Ann Thorac Surg 2011;92:1833-9.ArticlePubMed
- 5. Haghshenasskashani A, Rahnavardi M, Yan TD, McCaughan BC. Intrathoracic application of a vacuum-assisted closure device in managing pleural space infection after lung resection: is it an option? Interact Cardiovasc Thorac Surg 2011;13:168-74.ArticlePubMed
References
Figure & Data
References
Citations


 KSCCM
KSCCM
 PubReader
PubReader ePub Link
ePub Link Cite
Cite