Dear Editor:
Hypoxemic respiratory insufficiency resulting from severe acute respiratory syndrome coro- navirus 2 (SARS-CoV-2) infection might not be due to a “typical” acute respiratory distress syndrome (ARDS) [1]. As pulmonary compliance appears relatively preserved during the early stages of coronavirus disease 2019 (COVID-19), a role for right-to-left shunting due to pulmonary vasoplegia has been hypothesized, suggesting a possible therapeutic benefit from inhaled pulmonary vasodilators [1] including milrinone, nitric oxide, and cyclic prostaglandins (e.g., iloprost). Inhaled iloprost improves oxygenation in non–COVID-19 ARDS with minimal adverse effects, and has mitigating effects on microvascular thrombosis, endothelial injury, and pulmonary inflammation [2] in animal models of ARDS, suggesting potential beneficial effects on mechanisms behind lung injury in COVID-19 [3]. We introduced inhaled iloprost as a rescue therapy for patients with refractory hypoxemia due to COVID-19. Systemic and pulmonary hemodynamics were monitored using a pulmonary artery catheter (PAC).
The local Institutional Review Board approved this study (IRB No. 2021_071). Informed consent for the treatment was obtained.We present retrospective data from a single center (December 2020–May 2021). We hypothesized that inhaled iloprost improves oxygenation by causing preferential pulmonary vasodilatation, which decreases the shunt fraction. We included data from mechanically ventilated patients with COVID-19, severe ARDS according to the Berlin criteria, and oxygenation index [OI = (mean airway pressure×FiO2)/(PaO2, resures in mm Hg)] > 15 despite prone positioning, who were treated with iloprost, and in whom a PAC had been placed.
Iloprost (with a dose ranging 5–20 μg) was nebulized over 30 minutes and administered every 4 hours. The starting dose was 5 or 10 μg, which was increased on the basis of its clinical effects, up to a maximum of 20 μg. The effects on oxygenation were evaluated with arterial and mixed venous blood gas analyses. Samples were collected immediately before iloprost administration and then again at 30 and 60 minutes, and were repeated after any dose change. We calculated the right-to-left shunt fraction as follows:
, where Qs/Qt is the shunt fraction (percentage of cardiac out-put), and CaO2 and CvO2 are the arterial and mixed venous oxygen content, respectively.
Data are provided as median and interquartile range (IQR) or mean and standard deviation, and were compared using a paired t-test or Wilcoxon’s test, as appropriate (significance threshold, P<0.05).
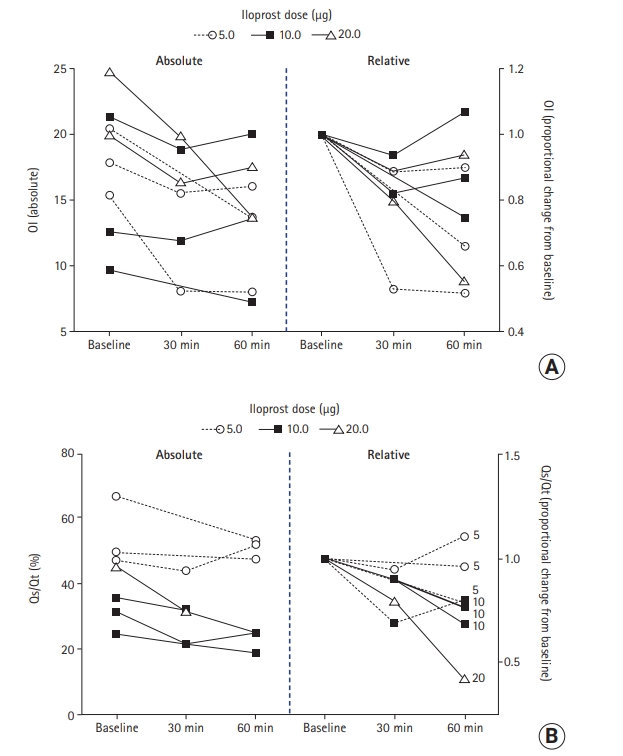
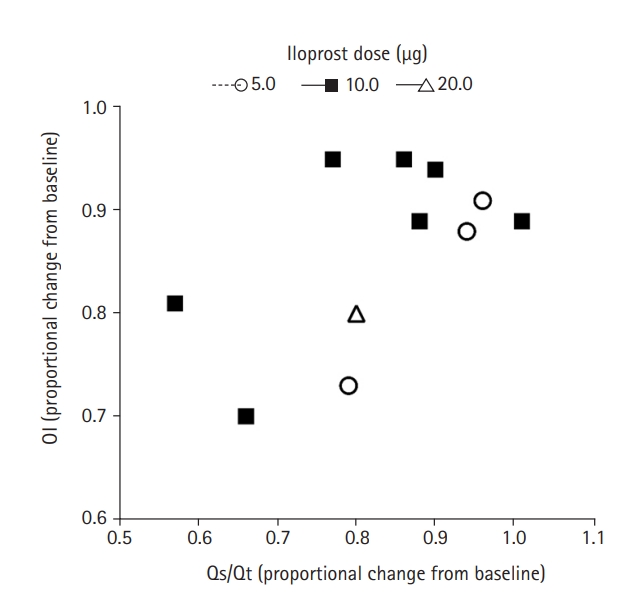
In total, eight patients met the inclusion criteria. Their median age was 72.5 years (IQR, 67.3–73.8 years); six patients were male. The median positive end-expiratory pressure was 12 cm H2O (IQR, 10−16 cm H2O); the median OI was 17.8 (IQR, 14.9−20.7), and the median PaO2 to FiO2 (P/F) ratio was 75.8 (IQR, 69.6–97.0). Iloprost was started at a median of 23 days (IQR, 14–29.5 days) after onset of symptoms and 12 days (IQR, 9−20 days) after intubation. Up to three measurement sets were performed per patient, resulting in a total of 18 (Table 1). When only the first set of measurements were considered for each patient (n = 8), the median P/F ratio increased from 75.8 to 96.0 mm Hg (IQR, 69.6–97.0 vs. 78.4–144.4; P=0.012), the mean OI decreased from 17.3 to 14.4 (P=0.007; absolute and relative changes are shown in Figure 1A), and the mean Qs/Qt decreased from 43.6% to 37.5% (P=0.025) (Figure 1B). Considering all sets of measurements, the median P/F ratio increased from 93.5 to 105.0 mm Hg ((IQR, 69.9–118.5 vs. 78.9–148.8; P<0.001), the mean OI decreased from 16.3 to 13.8 (P<0.001) (Supplementary Figure 1A), and the Qs/ Qt decreased from 44.2% to 36.9% (P=0.001) (Supplementary Figure 1B). The relationships between changes in Qs/Qt and OI are shown in Figure 2. Two patients developed transient hemodynamic side effects: one patient had a drop in systemic vascular resistance, while the other experienced a decrease in left ventricular preload, evidenced by decreased capillary wedge pressure.
Our findings provide proof-of-concept that inhaled iloprost can improve oxygenation by decreasing the shunt fraction in mechanically ventilated patients with severe COVID-19 ARDS. To our knowledge, the effects of inhaled iloprost on shunt fraction in severe COVID-19 have not been previously described. These effects of iloprost on oxygenation reflect those described by Sonti et al. [4] after administration of inhaled epoprostenol. However, shunt fraction was not reported, and Tsareva’s study [5] included measurements at widely varying intervals. Tsareva et al. [5] found improved oxygenation after 5 days of treatment with iloprost, suggesting a possible disease-modifying effect. However, their patients were not critically ill, and shunt fraction was not described.
Interestingly, right-to-left shunt fraction at baseline varied widely (19%–70%), possibly reflecting different disease phenotypes in COVID-19. Furthermore, although most patients showed improved oxygenation after administration of iloprost, some had only a relatively shortlived response, advocatingthe use of more frequent or continuous nebulization.
We used inhaled iloprost exclusively as a rescue therapy in patients in whom other interventions failed, which might have led us to include only the sickest patients. In such patients, consolidative and even fibrotic changes might have shown predominance over the vasculopathy that is thought to dominate hypoxemia in early COVID-19 (i.e., our patients might have already been in the H-stage, as proposed by Gattinoni et al. [1], wherein progressive parenchymal damage results in low compliance and a lesser role of vasoplegia).
From a pathophysiologic point of view, inhaled pulmonary vasodilators should have maximum effect during the L-stage, in which hypoxemia is thought to result primarily from ventilation/perfusion mismatch. Iloprost might have disease-modifying effects, by mediating platelet activation, endothelial damage, and pulmonary inflammation.
The retrospective nature of our study, its relatively small sample size, and the heterogenous patient population that received unequal doses in different phases of the disease preclude us from drawing conclusions about the magnitude of the effects of iloprost.
Future studies should aim to determine the category of COVID-19 patients that responds best to inhaled pulmonary vasodilators. In addition, measuring pulmonary hemodynamic parameters might contribute to further understanding of COVID-19 pathophysiology.
In conclusion, we found that inhaled iloprost can improve oxygenation in severe COVID-19 by decreasing shunt fraction. At baseline, shunt fraction varied widely, suggesting the existence of different mechanisms behind hypoxemia in severe COVID-19. Measuring the Qs/Qt should improve our understanding of refractory hypoxemia induced by SARS-CoV-2 and help tailor therapy for individual patients.
NOTES
-
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
Conceptualization: all authors. Data curation: CMCSAZ. Formal analysis: CMCSAZ. Methodology: all authors. Project administration: JLMLLN, CMCSAZ. Visualization: CMCSAZ. Writing–original draft: CMCSAZ, JlN. Writing–review & edit-ing: all authors.
Acknowledgments
We are grateful to our intensive care unit nurses, physicians and other staff. Without their help and expertise, the present study would not have been possible. We are specifically grateful for the contributions of Dr. O. Thomas in drafting the treatment protocol.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4266/acc.2021.01263.
Supplementary Figure
(A) The left panel depicts absolute changes in oxygenation index (OI), and the right panel depicts relative changes in OI after iloprost administration in eight patients with severe COVID-19. The X axis shows the timepoints at which measurements were performed as fol-lows: at baseline (n=17), before iloprost administration, and at 30 minutes (i.e., immediately after nebulization of the complete dose, n=11) and at 60 minutes after administration (n=15). The left Y axis shows absolute changes in OI. The right Y axis represents relative changes in OI compared with baseline (set to 1.0). Different symbols represent different dosages of iloprost administered (5 µg, 10 µg, and 20 µg). (B) The left panel depicts the absolute changes in shunt fraction (Qs/Qt) after iloprost administration in eight patients with severe coronavirus disease 2019 (COVID-19), and the right pan-el depicts relative changes. The X axis shows the timepoints at which measurements were performed as follows: at baseline (n=12), before iloprost administration, and at 30 minutes (i.e., immediately af-ter nebulization of the complete dose, n = 9) and at 60 minutes (n=11) after administration. The left Y axis demonstrates the change in Qs/Qt expressed in percentage. The right Y axis represents relative changes in Qs/Qt compared with baseline (set to 1.0). Different symbols represent different dosages of iloprost administered (5 µg, 10 µg, and 20 µg).
acc-2021-01263-suppl1.pdf
Figure 1.(A) The left panel depicts absolute changes in oxygenation index (OI), and the right panel shows relative changes in OI after iloprost administration in eight patients with severe coronavirus disease 2019 (COVID-19). A similar figure, including all measurements obtained, is presented in Supplementary Figure 1A. (B) The left panel depicts absolute changes and the right panel shows relative changes in shunt fraction (Qs/Qt) after iloprost administration in eight patients with severe COVID-19. A similar figure that includes all measurements obtained is shown in Supplementary Figure 1B. (A, B) Only measurements obtained around the first dose of iloprost received by each patient were included. The X axis shows the timepoints at which measurements were performed.
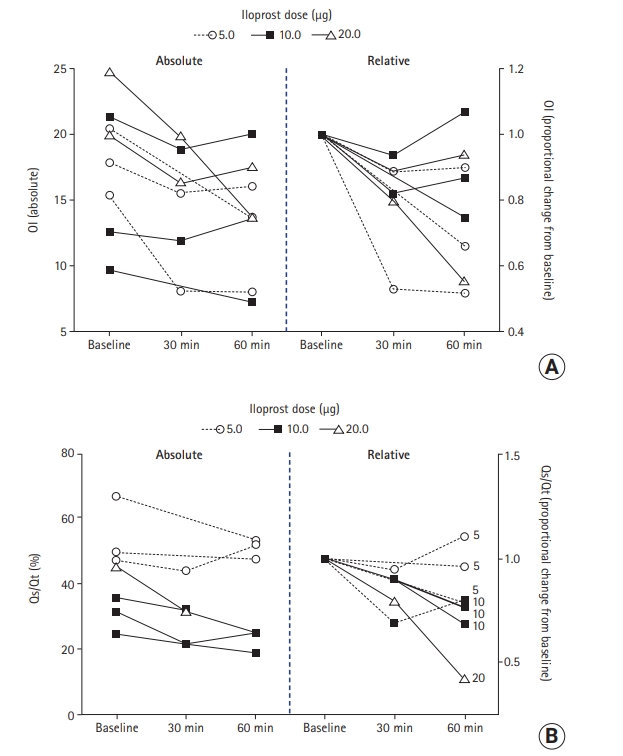
Figure 2.he relationship between changes in oxygenation index (OI) and shunt fraction (Qs/Qt) after iloprost administration in 11 measurements obtained in eight patients with severe coronavirus disease 2019 (COVID-19). X-axis and Y-axis include the first available measurement after administration of iloprost, expressed relative to the values obtained at baseline (which were set to 1.0).
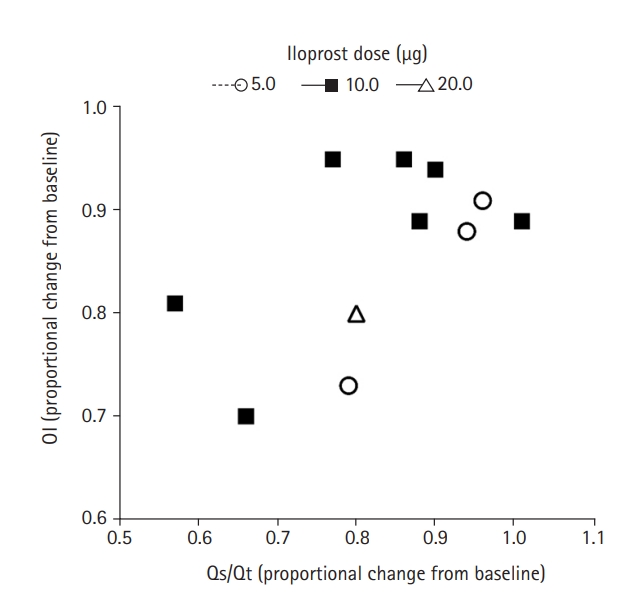
Table 1.Dosages received and number of measurements obtained for each patient
|
Patient |
Dose (μg) |
Measurement |
Note |
|
|
1 |
5, 10 |
2 |
|
|
|
2 |
10, 20 |
1 |
First dose (10 μg) given before placement of PAC because of acute and severe hypoxaemia; measurement performed around second dose (20 μg) |
|
|
3 |
5, 10 |
2 |
|
|
|
4 |
10 |
3 |
This patient had been in prone position for 13 days and desaturated upon multiple trials supine positioning. To allow for supine positioning, we started iloprost despite an initial OI of up to 10. |
|
|
5 |
20 |
2 |
Initial dose of 20 μg because of acute and severe hypoxaemia |
|
|
6 |
10, 20 |
3 |
|
|
|
7 |
5 |
2 |
|
|
|
8 |
10, 20 |
2 |
|
|
References
- 1. Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 Does not lead to a "typical" acute respiratory distress syndrome. Am J Respir Crit Care Med 2020;201:1299-300.Article
- 2. Riva CM, Morganroth ML, Ljungman AG, Schoeneich SO, Marks RM, Todd RF 3rd, et al. Iloprost inhib-its neutrophil-induced lung injury and neutrophil adherence to endothelial monolayers. Am J Respir Cell Mol Biol 1990;3:301-9.ArticlePubMed
- 3. Gu SX, Tyagi T, Jain K, Gu VW, Lee SH, Hwa JM, et al. Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation. Nat Rev Cardiol 2021;18:194-209.ArticlePubMed
- 4. Sonti R, Pike CW, Cobb N. Responsiveness of inhaled epoprostenol in respiratory failure due to COVID-19. J Intensive Care Med 2021;36:327-33.ArticlePubMed
- 5. Tsareva NA, Avdeev SN, Kosanovic D, Schermuly RT, Trushenko NV, Nekludova GV. Inhaled iloprost improves gas exchange in patients with COVID-19 and acute respiratory distress syndrome. Crit Care 2021;25:258. ArticlePubMedPMC
Citations
Citations to this article as recorded by

 , Norbert A. Foudraine1
, Norbert A. Foudraine1 , Jos L.M.L. Le Noble1,2
, Jos L.M.L. Le Noble1,2




 KSCCM
KSCCM
 PubReader
PubReader ePub Link
ePub Link Cite
Cite



