Current Status and Survival Impact of Infectious Disease Consultation for Multidrug-Resistant Bacteremia in Ventilated Patients: A Single-Center Experience in Korea
Article information
Abstract
Background
We evaluated the current status and survival impact of infectious disease consultation (IDC) in ventilated patients with multidrug-resistant (MDR) bacteremia.
Methods
One hundred sixty-one consecutive patients from a single tertiary care hospital were enrolled over a 5-year period. Patients with at least one of the following six MDR bacteremias were included: methicillin-resistant Staphylococcus aureus, extended-spectrum β-lactamase-producing gram-negative bacteria (Escherichia coli and Klebsiella pneumonia), carbapenem-resistant gram-negative rods (Acinetobacter baumannii and Pseudomonas aeruginosa), and vancomycin-resistant Enterococcus faecium.
Results
Median patient age was 66 years (range, 18 to 95), and 57.8% of subjects were male. The 28-day mortality after the day of blood culture was 52.2%. An IDC was requested for 96 patients based on a positive blood culture (59.6%). Patients without IDC had significantly higher rate of hemato-oncologic diseases as a comorbidity (36.9% vs. 11.5%, P < 0.001). Patients without an IDC had higher Acute Physiology and Chronic Health Evaluation (APACHE) II score (median, 20; range, 8 to 38 vs. median, 16; range, 5 to 34, P < 0.001) and Sequential Organ Failure Assessment (SOFA) score (median, 9; range, 2 to 17 vs. median, 7; range, 2 to 20; P = 0.020) on the day of blood culture and a higher 28-day mortality rate (72.3% vs. 38.5%, P < 0.001). In patients with SOFA ≥9 (cut-off level based on Youden’s index) on the day of blood culture and gram-negative bacteremia, IDC was also significantly associated with lower 28-day mortality (hazard ratio [HR], 0.298; 95% confidence interval [CI], 0.167 to 0.532 and HR, 0.180; 95% CI, 0.097 to 0.333; all P < 0.001) based on multivariate Cox regression analysis.
Conclusions
An IDC for MDR bacteremia was requested less often for ventilated patients with greater disease severity and higher 28-day mortality after blood was drawn. In patients with SOFA ≥9 on the day of blood culture and gram-negative bacteremia, IDC was associated with improved 28-day survival after blood draw for culture.
Introduction
The incidence of serious infectious complications caused by multidrug-resistant (MDR) bacteria has been increasing in intensive care unit (ICU) patients [1], resulting in high rates of morbidity and mortality, high costs, and longer hospital stays [2,3]. Therefore, reducing the occurrence of MDR bacterial infections has become a major objective for many hospitals because it will improve patient outcome and reduce the financial burden [2,4]. Among the important steps cited in published recommendations regarding the rational use of antibiotics are a reduction in the duration of empirical broad-spectrum antibiotic therapy and the timely use of more appropriate antibiotics [5-7].
A further step is the establishment of a hospital team that includes an infectious disease (ID) specialist [5]. The assessment by an ID physician of antibiotic use in patients can result in significant improvements in the prescription of antibiotics, decreased antibiotic consumption, and lower mortality and readmission rates [8,9]. Indeed, active intervention by ID specialists in ventilated patients with infectious complications aids critical care physicians in managing patients with MDR bacterial infections and may improve patient outcomes.
In Korea, however, critical care delivery systems are underdeveloped compared to those in Western countries [10,11]. Few hospitals have established local teams with ID specialists, clinical microbiologists, clinical pharmacists, and infection control practitioners specialized in care of ICU patients. In contrast, many hospitals are dependent on formal consultations with ID specialists in the management of ICU patients with newly developed infectious complications. The utility of these consultations in patients with MDR bacteremia has yet to be evaluated. Also, it is questionable whether specialist consultation (infectious disease consultation [IDC]) is more useful in patients with higher severity illness and organ failure than in patients with lower severity illness. To address this issue, we investigated the current status of IDC for ventilated patients with MDR bacteremia. We also examined the effects of IDC on the survival of these patients in an acute care hospital in Korea.
MATERIALS AND METHODS
Study Design, Ethics, and Subject Selection
This retrospective study included all consecutive patients who had positive blood culture tests and who required ventilator care while hospitalized in the ICU of Pusan National University Hospital between March 2011 and February 2016. This hospital has six functionally separate ICUs with a total of 85 beds (medical, 12 beds; surgical, 10 beds; cardio-stroke, 14 beds; neurosurgical, 13 beds; emergency, 20 beds; and trauma, 16 beds). All have full cardiovascular and close airway monitoring equipment. Each has one full-time ICU specialist; the nurse-tobed ratio is 1 : 3. All patients are managed according to therapeutic recommendations based on current sepsis guidelines and a lung-protective ventilator strategy [12,13].
During the study period, two or three board-certified ID specialists provided bedside consultations in the ICUs. These were performed only upon request from the primary treating physicians, who contacted the covering specialists via electronic medical records or telephone. ID specialists were available Monday through Friday during normal working hours, but were typically not available during the night or on weekends.
Our study was approved by the Institutional Review Board of Pusan National University Hospital (IRB No. H-1707-011-057). The need for informed consent from patients was waived due to the observational and retrospective nature of this study. All investigators contributed to the design of the study and confirmed that the study objectives and procedures were honestly disclosed. Between November 2016 and May 2017, the electronic medical records of all enrolled patients were reviewed retrospectively. Relevant medical, laboratory, and radiological data were extracted and used to complete a case report form for each patient. The data in these reports were analyzed. Our study had no impact on the treatment of patients in the study.
In the present study, all ICU adult patients (≥18 years of age) were screened if they had received ventilator care and had a positive blood culture during the study period. Patients with one of the following six MDR bacteremias were included: methicillin-resistant Staphylococcus aureus (MRSA), extended-spectrum β-lactamase (ESBL)-producing gram-negative bacteria (Escherichia coli and Klebsiella pneumonia), carbapenem-resistant gram-negative rods (Acinetobacter baumannii [CRAB] and Pseudomonas aeruginosa [CRPA]), and vancomycin-resistant Enterococcus faecium (VRE). Patients with a second bacteremia episode within 3 days after the first (index) one were excluded. For all positive blood cultures, organisms were identified by conventional and automated biochemical methods (VITEK 2; BioMérieux, Marcy l’Étoile, France) from March 2011 to February 2013 and by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS; Bruker Daltonic, Bremen, Germany) from March 2013 to February 2016.
Data Collection
The following demographic and clinical data were gathered from the medical records of each patient: age, sex, comorbidities before ICU admission, length of ICU stay and hospital stay, and ventilator care. The severity of illness was measured using the Acute Physiology and Chronic Health Evaluation (APACHE) II score, and accompanying organ failure was assessed according to the Sequential Organ Failure Assessment (SOFA) score [14,15]. APACHE II and SOFA scores were calculated based on laboratory and clinical data recorded on the day of blood culture collection. Requirement for hemodialysis (defined as the use of any form of renal replacement therapy), neuromuscular blocking agents, and vasopressors on the day of blood culture collection were also noted.
Microbiological information for each MDR bacterium, including its identification and antimicrobial susceptibility test results, was obtained from medical records. The primary source of infection upon ICU admission was also recorded. Whether an ID specialist was consulted based on the identified microorganisms was also evaluated. Empirical antibiotic use for >3 days prior to blood sampling was documented in all patients. Adjusted antibiotics used for >3 days based on the microorganisms identified in the blood culture, regardless of IDC, were also recorded for all patients.
In this study, an IDC was defined as the first formal ID consultation, regardless of the eventual final number of consultations, as documented in the patient’s medical records within 3 days after the final microbiological determination. Survivors were defined as patients who survived for 28 days after blood was drawn.
Statistical Analysis
Continuous variables are expressed as median and range; categorical variables are presented as number and percent. Student t-test or the Mann-Whitney U-test was used to compare continuous variables, and the chi-square or Fisher exact test (for small numbers) was used to compare categorical variables. Receiver operating characteristic curves and the area under the curve (AUC) were used, and identification of an optimal cut-off value for the SOFA score was based on the maximum Youden’s index [16]. Univariate Cox proportional hazard models were developed to determine the relationship between ID consultation, other clinical variables, and 28-day mortality. Variables with P < 0.1 were included in multivariate Cox proportional hazard models. Backward elimination was performed to eliminate any predictor for which the P-value of the multivariate model exceeded 0.05. Hazard ratios with 95% confidence intervals are reported. All tests of significance were two-tailed, and P-values <0.05 were considered significant. Our statistical analysis was supported by our hospital biostatistics office. All analyses were performed using IBM SPSS version 24.0 (IBM Corp., Armonk, NY, USA) and MedCalc Statistical Software version 17.9.7 (MedCalc Software, Ostend, Belgium).
RESULTS
Baseline Characteristics
Among the 1,283 ICU patients with positive blood cultures during the study period, 161 were eligible for participation in the study. Blood for microorganism culture was collected a median of 9 days (range, 0 to 413) after ICU admission. The median time from blood collection to microorganism identification and antibiotic susceptibility testing was 89 hours (range, 44 to 695). Respiratory infections were the most common source of bacteremia (47.2%), and MRSA and CRAB were the most commonly identified microorganisms in these infections (36.6%) (Table 1). Two or more microorganisms were identified in the blood cultures of eight patients. The 28-day mortality rate was 52.2%.
ID Specialist Consultation Activity
IDC was requested for positive blood culture results in 96 patients (59.6%). Table 1 compares the clinical parameters of the IDC and no-IDC groups. Patients who received IDC had a higher rate of catheter-related infections. All patients in the trauma ICU had IDC for positive blood culture results. Patients without IDC had higher APACHE II and SOFA scores on the blood culture day, but also significantly higher rates of hemato-oncologic diseases as a comorbidity, greater requirements for vasopressors and hemodialysis on the blood culture day, and higher 28-day mortality. Also, patients who received IDC had significant alterations to the first recommended antibiotic for MDR bacteria and were prescribed these antibiotics for a significantly longer period (Table 1). Among the patients who underwent IDC, 39 (40.6%) had their antibiotics changed to the recommended antibiotics based on MALDI-TOF MS results (only pathogen identification), while 16 patients (16.7%) had their antibiotics changed based on the final drug susceptibility test.
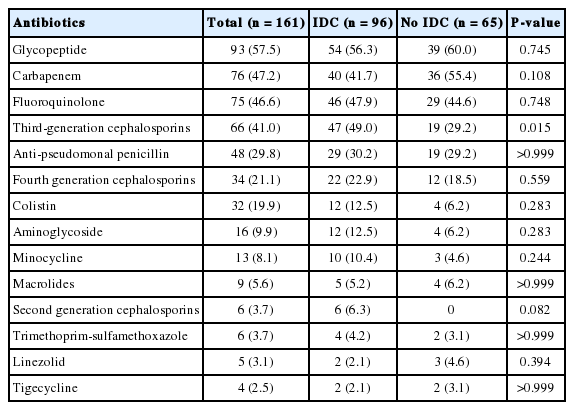
Table 2 shows the antibiotics used for more than 3 days before blood was drawn in all patients. Glycopeptide, carbapenem, fluoroquinolone, and third-generation cephalosporins were the most common antibiotics used in both groups of patients. Antibiotics were adjusted in 79 patients (49.1%) based on microorganism identification and antimicrobial susceptibility test results. Table 3 lists the adjusted antibiotics for the two groups according to identified microorganism. In patients with ESBL-producing gram-negative bacteremia, carbapenem was used significantly more in the IDC group. In patients with carbapenem-resistant gram-negative rods bacteremia, the proportion of colistin or minocycline use was higher in the IDC group, whereas fluoroquinolone and third-generation cephalosporins were more frequently used in the no-IDC group. In patients with MRSA bacteremia, there was no significant difference between the two groups. In those with VRE bacteremia, glycopeptide use was significantly higher in the no-IDC group than the IDC group.
Effect of IDC on Clinical Outcomes
Univariate and multivariate Cox regression models were constructed to evaluate the influence of IDC on survival in all patients (Table 4). IDC showed a significant association with survival. The Kaplan-Meier estimate of survival at 28 days was consistent with a survival benefit of IDC (Figure 1). However, requirement for vasopressors, hemodialysis, and neuromuscular blocking agents and thrombocytopenia on the day of blood culture were associated with 28-day mortality. Subgroup analysis was performed to determine whether the higher 28-day mortality in the no-IDC group biased the influence of IDC on survival. To evaluate the influence of IDC in more seriously ill patients, we assessed how APACHE II and SOFA predicted 28-day mortality. We found that the AUC for the SOFA score was significantly higher than that for the APACHE II score (AUC, 0.747; 95% confidence interval [CI], 0.673 to 0.813 vs. AUC, 0.708; 95% CI, 0.632 to 0.777; P = 0.039) (Figure 2). Furthermore, the cut-off SOFA score was 9 based on Youden’s index (sensitivity 88%, specificity 56%). In subgroup analysis of patients with SOFA score ≥9, IDC was significantly associated with survival based on multivariate Cox regression analysis (Table 4). In patients with gram-negative bacteremia (ESBL-producing and carbapenem-resistant gram-negative bacteremias), multivariate analysis showed that IDC was also significantly associated with improved survival. However, there was no association between IDC and survival in patients with MRSA or VRE bacteremia (Table 4).
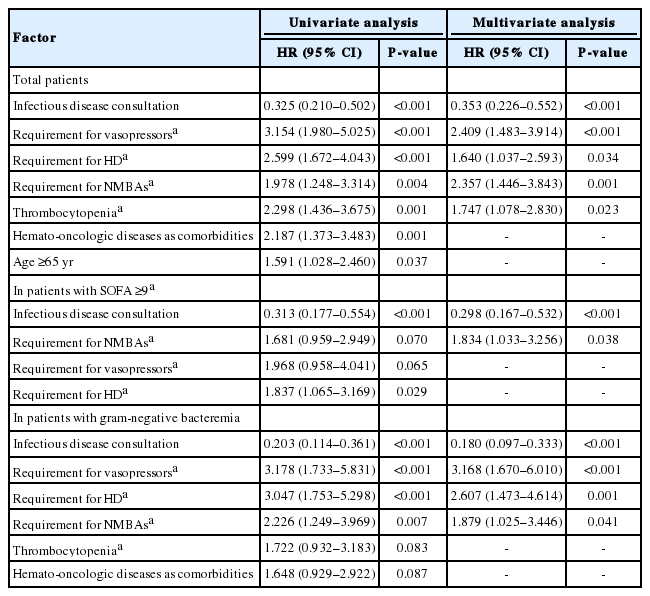
Univariate and multivariate analysis of factors associated with 28-day mortality after blood was drawn in total patients and some subgroups

Kaplan-Meier curves of survival 28 days after the day of blood culture according to the presence or absence of infectious disease consultation (log-rank, 29.507, P < 0.001). ICU: intensive care unit.
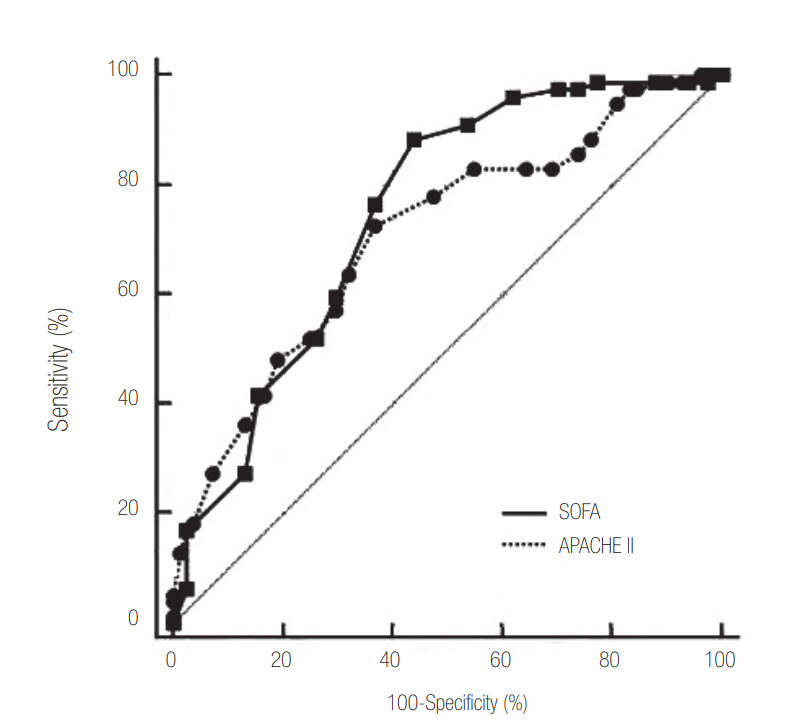
Receiver operating characteristic curves for SOFA and APACHE II scores on the day of blood culture collection predicting 28-day mortality after blood was drawn. AUC for SOFA was 0.747 (95% CI, 0.673 to 0.813) vs. APACHE II with an AUC of 0.708 (95% CI, 0.632 to 0.777) (P = 0.039). SOFA: Sequential Organ Failure Assessment; APACHE: Acute Physiology and Chronic Health Evaluation; AUC: area under the curve; CI: confidence interval.
DISCUSSION
We found that roughly 60% of our 161 enrolled patients received IDC services for selection of optimal antibiotics despite the high 28-day mortality in our series. Univariate analysis of patients with a SOFA score ≥9 on the day of blood culture collection showed that IDC was associated with reduced mortality, which suggests that IDC could improve the outcome of patients who are severely ill and have organ failure. However, IDC services were requested less often for patients with greater disease severity and mortality. Moreover, broad-spectrum antibiotics were still used before and after microorganism identification regardless of IDC, as shown in Table 3.
Reduced in-hospital mortality and decreased overall hospital costs associated with IDC have been described in several studies [9,17-21]. In addition, antimicrobial stewardship has been recognized internationally as a key strategy to address the global crisis of escalating antimicrobial resistance [22,23]. Despite increasing consumption of empirical broad-spectrum antibiotics in many Korean university-affiliated hospitals, there are few established antimicrobial stewardship programs in our country. Our present study results emphasize the importance of IDC in MDR bacteremia to prevent serious complications and improve patient outcomes. Antibiotics stewardship programs need to be introduced to control the increasing prevalence of MDR bacteria in South Korea.
In the present study, we showed that IDC was associated with a reduction in mortality due to gram-negative bacteremia. Previous data on the clinical utility of IDC in patients with S. aureus bacteremia suggest that IDC may be particularly beneficial in patients with MRDA bacteremia [17,18,24-26]. However, our data do not indicate that IDC had a clinical impact on mortality in patients with MRSA. More than half of all enrolled patients received glycopeptides as empirical antibiotics before microorganism identification (Table 2). Moreover, patients with MRSA bacteremia had a lower 28-day mortality rate than did patients with other MDR bacteremias (33.9% vs. 62.7%, P = 0.001). Although our data suggest that IDC is less useful in patients with MRSA bacteremia, further studies are required to determine the clinical utility of IDC according to the identified microorganism, which was not possible in this study because of the small sample size.
Our study had several limitations. First, even though IDC was associated with reduced mortality in patients who were more severely ill, we could not unambiguously demonstrate the clinical utility of IDC in reducing mortality, because patients in the IDC group had significantly lower APACHE II and SOFA scores than those in the no-IDC group. Second, this study had a retrospective design, which may have resulted in selection bias. In addition, our enrolled patient populations were heterogeneous as they were hospitalized in six ICUs at our hospital, which may have been a source of bias. Furthermore, it was not possible to control for other confounding variables affecting outcomes because of our study’s retrospective cohort design. Last, because our data represent the experience of a single center and the sample size was small, the results may not be representative of the general situation in Korea.
In conclusion, our analysis showed that IDCs were requested less often for ventilated patients with documented MDR bacteremia than for those with high APACHE II and SOFA scores on blood-collection day. Furthermore, IDC was associated with improved outcomes in patients with higher severity illness than those with lower severity illness. Given the increased incidence of MDR bacteria in the ICU, ID specialists have an important role to play in the control of undisciplined use of broad-spectrum antibiotics. Further large-scale studies are required to determine the role of ID specialists in controlling MDR bacteria in the ICU.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean Government (Ministry of Science and ICT) (2016R1C1B1008529).