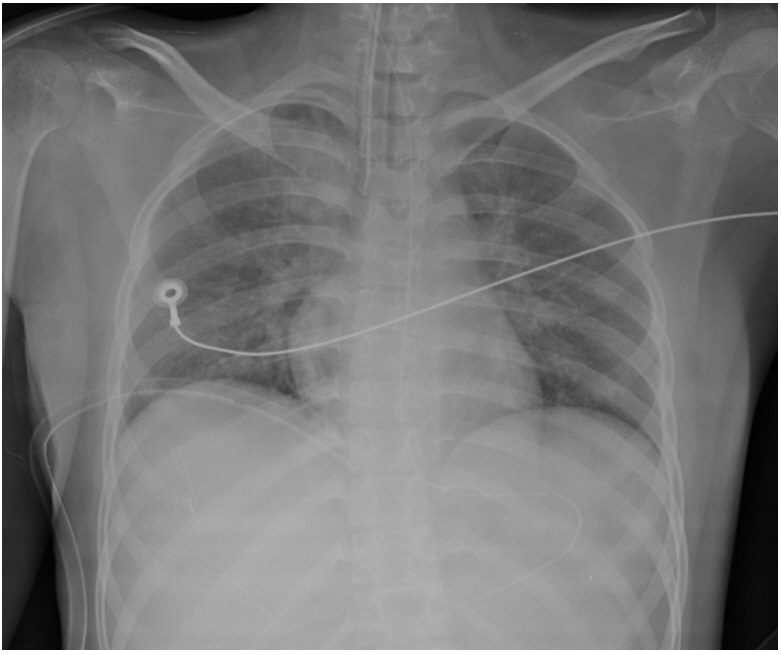
Tension Pneumothorax after Attempting Insertion of a Central Venous Catheter
Article information
A 17-year-old female patient was admitted to the emergency department of our hospital with dyspnea, which had presented 1 day earlier but had worsened despite treatment at another hospital. Before the onset of dyspnea, she had been undergoing follow-up in our pediatrics department because of repetitive aspiration pneumonia associated with cerebral palsy. On admission, her vital signs revealed a blood pressure of 60/40 mmHg, a temperature of 38°C, and a heart rate of 185 bpm. Arterial blood gas analysis showed pH 7.09, pCO2 67 mmHg, pO2 53 mmHg, and O2 saturation 72%. Central venous catheterization was attempted under mechanical ventilation into the right subclavian vein without success. While undergoing another catheterization into the left subclavian vein, the patient went into cardiac arrest and required cardiopulmonary resuscitation (CPR). Spontaneous circulation returned 5 minutes after CPR, but a right-sided tension pneumothorax was detected on chest radiography (Figure 1). After a thoracostomy was performed, her tension pneumothorax improved immediately (Figure 2). The patient was transferred to an intensive care unit because of sepsis resulting from aspiration pneumonia. The chest tube was removed 4 days after placement, and the patient was discharged 40 days after admission.

Chest X-ray showing right tension pneumothorax with mediastinal shifting to the left side. The right lung is completely collapsed (arrows), and the trachea is pushed to the left. The right hemidiaphragm is depressed.
Pneumothorax is the one of the most frequent complications during central venous catheterization, especially after subclavian vein catheterization [1,2]. Tension pneumothorax occurs due to progressive accumulation of intrapleural air in the thoracic cavity caused by a valve effect during respiration. Positive pressure ventilation may exacerbate a tension pneumothorax [3,4]. Progressive increased intrathoracic pressure in the pleural space pushes the mediastinum to the opposite hemithorax and obstructs venous return to the heart. This leads to circulatory instability and may result in cardiorespiratory arrest. To prevent life-threatening situations caused by tension pneumothorax, it is important to detect these occurrences early and decompress them quickly.