Impact of Socioeconomic Status on 30-Day and 1-Year Mortalities after Intensive Care Unit Admission in South Korea: A Retrospective Cohort Study
Article information
Abstract
Background
Socioeconomic status (SES) is closely associated with health outcomes, including mortality in critically ill patients admitted to intensive care unit (ICU). However, research regarding this issue is lacking, especially in countries where the National Health Insurance System is mainly responsible for health care. This study aimed to investigate how the SES of ICU patients in South Korea is associated with mortality.
Methods
This was a retrospective observational study of adult patients aged ≥20 years admitted to ICU. Associations between SES-related factors recorded at the time of ICU admission and 30-day and 1-year mortalities were analyzed using univariable and multivariable Cox regression analyses.
Results
A total of 6,008 patients were included. Of these, 394 (6.6%) died within 30 days of ICU admission, and 1,125 (18.7%) died within 1 year. Multivariable Cox regression analysis found no significant associations between 30-day mortality after ICU admission and SES factors (P>0.05). However, occupation was significantly associated with 1-year mortality after ICU admission.
Conclusions
Our study shows that 30-day mortality after ICU admission is not associated with SES in the National Health Insurance coverage setting. However, occupation was associated with 1-year mortality after ICU admission.
INTRODUCTION
Socioeconomic status (SES) is a total measure of an individual’s social and economic statuses and includes income level, education level, and occupation [1]. SES is known to be related to patients’ health conditions [2]. Inequality in SES can cause differences in mortality rates [3], making it an important public health issue worldwide [3-5].
In critically ill patients, admission to the intensive care unit (ICU) plays an important role in determining hospital mortality [6]. One of the most important factors associated with the mortality of patients admitted to ICU is a low SES score [7,8]. In addition, insurance coverage in each society and country has been recognized as an important SES factor leading to differences in outcomes. A study conducted in the United States reported that there was a difference in mortality among ICU patients depending on insurance status and coverage types [9]. However, although it is highly possible that the differences in treatment outcomes according to SES or insurance status in patients in ICUs are due to the differences in the health care systems between countries and societies, most cohort studies have been based in the United States [9-11].
In South Korea, patients, including those who are critically ill, can benefit from National Health Insurance when undergoing treatment or surgery [12]. South Korea is also associated with an intense fervor for education [13]. Recently, it was reported that in South Korea, patients’ SES before surgery is associated with 30-day and 1-year mortalities after surgery, with marital status correlating with increased mortality [14]. However, there are no studies reporting the association between SES at the time of ICU admission and mortality rate after ICU admission conducted in Asia, including South Korea. Therefore, we conducted this study with the aim of investigating the association between patients’ SES and their 30-day and 1-year mortalities after ICU admission in South Korea, where National Health Insurance is compulsory.
MATERIALS AND METHODS
The present retrospective observational study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-1804/462-104, approval date: April 13, 2018). Considering the retrospective design of this study, the IRB waived the requirement for informed consent. This study analyzed the medical records of patients aged ≥20 years who were admitted to four ICUs (medical ICU, neurologic ICU, emergency ICU, and surgical ICU) between January 1, 2012, and July 31, 2016. Patients with inaccurate or no medical records were excluded. For patients with ≥2 ICU admissions, only the last admission was included in the analysis.
ICU Staffing from 2012 to 2016
During the research period, high-intensity day-time (8:00 AM–6:00 PM) staffing was executed in each ICU by day-time intensivists (anesthesiologists, pulmonologists, neuro-intensivists, thoracic surgeons), who were responsible for providing patient care in ICUs. On weekends, or during weekday night times, intensivists were on-call; they took calls related to patient severity and procedures. Second- and third-year residents provided the main patient care in ICUs.
Measurements and Outcomes
The following data were collected from medical records for this research: (1) demographic data (sex/body mass index [BMI, kg/m2]/age [year]); (2) alcohol use (non-alcohol user/current alcohol user/former alcohol user) and smoking status (never smoker/current smoker/former smoker); (3) clinical characteristics (Acute Physiology and Chronic Health Evaluation [APACHE] II score, Charlson comorbidity index score, postoperative ICU admission, diagnosis of cancer, length of hospital and ICU stay [day], year of ICU admission, death dates); (4) SES factors (educational level [less than high school/more than or equal to high school/less than college/more than or equal to college], occupation at ICU admission [office worker/professional job/housework/self-employed/student/military/day labor/unemployed], marital status [never married/married, live together/divorced, separated/widowed], religion [Protestant/Catholic/Buddhism/others, e.g., Hinduism, Islam, Chondogyo]), and if the patient belonged to the medical protection group according to the insurance system.
A patient was defined as unemployed when there was no record of a specific job just before entering the ICU. Current smoker or alcohol users were those with a history of smoking or alcohol consumption within 1 month from ICU admission. Medical protection patients are the medically vulnerable officially registered with the National Health Insurance System in South Korea. SES-related information was based on initial nursing information records that were completed either by the patient or their legal guardians at the time of ICU admission. Patients were allowed to refuse disclosure of information regarding their SES. Data regarding the date of death, including those patients who were unavailable for follow-up, were accurately collected after receiving an approval from the Ministry of the Interior and Safety of South Korea. All other data were collected by medical record technicians from medical informatics teams who were blinded to the purpose of the study. The primary aim of this study was to investigate if there are differences in 30-day and 1-year mortalities after ICU admission according to the SES of patients at the time of ICU admission.
Statistical Method
All patients’ baseline characteristics were expressed as numbers with percent or mean with standard deviation. A univariable Cox regression analysis was performed to analyze the simple relationship between 30-day mortality after ICU admission, and each variable. From the univariable Cox regression model, covariates (not SES-related factors) with P<0.1, and all reselected main independent SES-related variables were included in the final multivariable Cox regression analysis. Univariable and multivariable Cox regression analyses were also used for 1-year mortality after ICU admission. In addition, a Kaplan-Meier curve of overall survival time according to occupation post ICU admission was generated after adjustment of covariates with the criterion of P<0.05 in multivariable Cox regression analysis for 1-year mortality. All analyses were performed using IBM SPSS version 24.0 software (IBM Corp., Armonk, NY, USA).
RESULTS
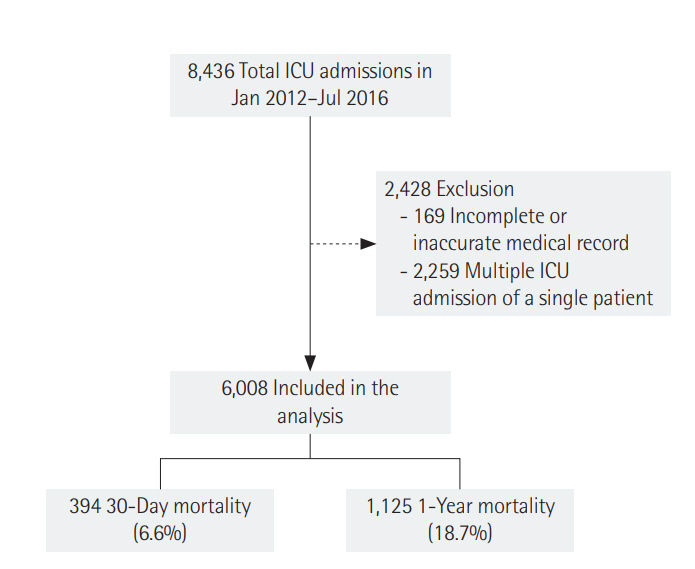
A total of 8,436 cases of ICU admission among adults aged ≥20 years were recorded between January 2012 and July 2016. Of these, 169 cases were excluded due to missing or inaccurate SES-related information. Of the remaining 8,267 cases, 2,259 cases who were admitted to an ICU twice or more were also excluded. A total of 6,008 patients were included in the final analysis. Of these, 394 patients (6.6%) died within 30 days of ICU admission, and 1,125 patients (18.7%) died within 1 year of ICU admission (Figure 1). Table 1 shows the baseline characteristics of these patients.
30-Day and 1-Year Mortalities after ICU Admissions According to SES
Supplementary Tables 1 and 2 show the results of univariable Cox regression analysis for 30-day and 1-year mortalities, respectively. Tables 2 and 3 show the results of multivariable Cox regression analyses on 30-day mortality and 1-year mortality after ICU admission, respectively. In the multivariable Cox regression analysis, none of the SES-related factors were significantly associated with 30-day mortality (P>0.05). However, occupation at the time of ICU admission was significantly associated with 1-year mortality after ICU admission in the multivariable Cox regression analysis. Of the different occupations, housework was significantly associated with a 53% increase in 1-year mortality after ICU admission compared with office work (hazard ratio [HR], 1.53; 95% confidence interval [CI], 1.10 to 2.12; P=0.012). The self-employed group was significantly associated with a 42% increase (HR, 1.42; 95% CI, 1.01 to 1.99; P=0.042), student and military or day labor groups were associated with a 45% increase (HR, 1.45; 95% CI, 1.06 to 2.00; P=0.021), and the unemployed group was associated with an 83% increase (HR, 1.83; 95% CI, 1.37 to 2.43; P<0.001) in 1-year mortality following ICU admission. Figure 2 shows Kaplan-Meier curve of overall survival after ICU admission with adjustment for covariates in the multivariable Cox regression model for 1-year mortality (P<0.05) and shows similar tendency to multivariable Cox regression analysis for 1-year mortality.
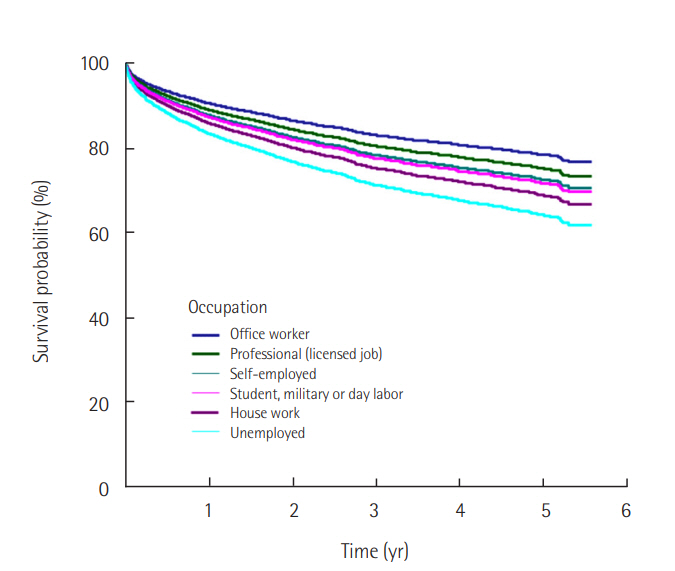
Kaplan-Meier curve of overall survival time according to occupation after adjustment of covariates with criterion of P<0.05 in multivariable Cox regression analysis for 1-year mortality. Included covariates are sex, age, body mass index, Charlson comorbidity index, Acute Physiology and Chronic Health Evaluation II, diagnosis of cancer, postoperative intensive care unit (ICU) admission and year of ICU admission.
DISCUSSION
This study demonstrates that SES at the time of ICU admission is not independently associated with 30-day mortality after ICU admission, whereas occupation at the time of ICU admission is associated with 1-year mortality. These results are meaningful as they were adjusted for various demographic and clinical factors including sex, age, BMI, cancer, Charlson comorbidity index, APACHE II, and year of ICU admission. This study being conducted in an ICU setting, it is notable in that its findings differ from those of previous research in which we reported that marital status, not occupation, is usually associated with 30-day and 1-year mortalities [14].
The main finding of the present study that occupation at ICU admission was associated with 1-year mortality, not 30-day mortality, may be explained by certain factors. Firstly, 1-year mortality may reflect long-term mortality for ICU survivors, while 30-day mortality may reflect hospital mortality. Secondly, in critically ill patients, lower SES is known as an associated factor affecting relative long-term mortality rather than short-term mortality [15]. In addition, a study from South Korea has reported that an office worker undergoes more health check-ups compared to a manual worker [16]. Therefore, the difference in HR of 1-year mortality may be affected by the difference in routine health check-up except for those in professional jobs. Furthermore, there is a possibility that patients who are unemployed and who showed the highest HR in 1-year mortality, could not work due to severe chronic illness such as cancers, at the time of ICU admissions. Therefore, careful interpretation is required to understand the results of the present study.
The present study is meaningful in that it is a cohort study conducted in a setting where the entire nation receives similar benefits from the National Health Insurance system of South Korea with a low financial burden [17]. According to a study conducted in the United States, where private health insurance systems play an important role [18], lack of health insurance increased 30-day mortality after ICU admission. Although there is also a report that expansion of Medicaid services for patients with low income and resources improved mortality in the United States [19], critically ill patients who only have public health insurances still have higher mortality rates than those who have additional private health insurances in the United States [9]. In other words, contrary to South Korea, where all patients receive similar treatments in ICUs through the National Health Insurance Services, in the United States, the type of health insurance one holds is the most important SES-related factor that determines mortality in ICU patients. As such, our study greatly differs from these American studies.
There are countries such as Canada and the United Kingdom where similar to South Korea, the National Health Insurance System is responsible for providing the main health care including ICU care [20]. Regarding previous studies on the association between mortality in ICUs and SES in these countries, one study has reported that a higher SES is associated with lower mortality in the case of elective surgical ICU admission in England and Wales [7]. In countries where a national health insurance system is established, other SES factors, aside from health insurance status, may be independently associated with the mortality of ICU patients, and this study shows that occupation is associated with 1-year mortality.
Another interesting finding of this study is that in the National Health Insurance coverage setting, different results were obtained between 30-day and 1-year mortalities after ICU admission. Firstly, 30-day mortality shares similarities with hospital mortality, which reflects on the health care in ICUs [21]. The fact that 30-day mortality after ICU admission was not independently associated with SES suggests that all patients admitted to ICUs received the same treatment under the National Health Insurance scheme regardless of their SES. In addition, the medical protection patient did not show worse 30-day or 1-year mortality after ICU admission, which means the National Health Insurance System supports the economically disadvantaged patients effectively.
Secondly, 1-year mortality after ICU admission is a longterm outcome measure for patients who were critically ill, and SES-related factors may have also affected 1-year mortality. For example, in Canada, where the National Health Insurance System plays the main role in health care, similar to South Korea, Canadians of upper middle SES were more likely to be prioritized in their access to the health care system [22]. Therefore, one of the factors explaining our finding suggests that there may be differences in the level of healthcare access according to SES among ICU patients in South Korea as is the case in Canada. Further research from the perspective of public health care is needed in this regard.
Another point to note is that our results in the general surgical population differed from those of a previous cohort study [14], which reported increased 30-day and 1-year mortalities in the never-married group following surgery, with occupation not affecting mortalities. Such a difference may be attributed to the different characteristics of the two patient groups. In this study, most subjects were critically ill patients with relatively old age and high Charlson comorbidity indices.
This study has a number of limitations. First, due to the limitation of the retrospective cohort design, there may have been a selection bias. However, to prevent such bias, we had medical record technicians blinded from the purpose of this study and the main researchers were also blinded from data until all statistical outcomes were obtained. Second, due to the nature of a cohort study based on 5 years of medical records from a single tertiary care hospital, we cannot generalize the findings from ICUs to all Korean hospitals. Finally, although we had accurate information regarding the date of death of all patients, it was hard to find the causes of death. It was therefore not possible to investigate disease-specific mortality. Despite these limitations, this study is meaningful in that it is the first study to analyze the association between SES factors and 30-day and 1-year mortalities in patients in South Korea where the National Health Insurance System plays the main role in health care.
In conclusion, this study shows that 30-day mortality after ICU admission is not associated with patients’ SES in the National Health Insurance coverage setting, while 1-year mortality after ICU admission is associated with occupation.
KEY MESSAGES
▪ Socioeconomic status at the time of intensive care unit (ICU) admission is not independently associated with 30-day mortality after ICU admission, whereas occupation at the time of ICU admission is associated with 1-year mortality.
Notes
No potential conflict of interest relevant to this article was reported.
SUPPLEMENTARY MATERIALS
The online-only Supplement data are available with this article online: https://doi.org/10.4266/acc.2018.00514.