The Adequacy of a Conventional Mechanical Ventilator as a Ventilation Method during Cardiopulmonary Resuscitation: A Manikin Study
Article information
Abstract
Background
We conducted this study to verify whether a mechanical ventilator is adequate for cardiopulmonary resuscitation (CPR).
Methods
A self-inflating bag resuscitator and a mechanical ventilator were used to test two experimental models: Model 1 (CPR manikin without chest compression) and Model 2 (CPR manikin with chest compression). Model 2 was divided into three subgroups according to ventilator pressure limits (Plimit). The self-inflating bag resuscitator was set with a ventilation rate of 10 breaths/min with the volume-marked bag-valve procedure. The mode of the mechanical ventilator was set as follows: volume-controlled mandatory ventilation of tidal volume (Vt) 600 mL, an inspiration time of 1.2 seconds, a constant flow pattern, a ventilation rate of 10 breaths/minute, a positive end expiratory pressure of 3 cmH2O and a maximum trigger limit. Peak airway pressure (Ppeak) and Vt were measured by a flow analyzer. Ventilation adequacy was determined at a Vt range of 400-600 mL with a Ppeak of ≤ 50 cmH2O.
Results
In Model 1, Vt and Ppeak were in the appropriate range in the ventilation equipments. In Model 2, for the self-inflating bag resuscitator, the adequate Vt and Ppeak levels were 17%, and the Ppeak adequacy was 20% and the Vt was 65%. For the mechanical ventilator, the adequate Vt and Ppeak levels were 85%; the Ppeak adequacy was 85%; and the Vt adequacy was 100% at 60 cmH2O of Plimit.
Conclusions
In a manikin model, a mechanical ventilator was superior to self-inflating bag resuscitator for maintaining adequate ventilation during chest compression.
Introduction
Although ventilation plays an important role in high quality cardiopulmonary resuscitation (CPR), it is difficult to perform appropriate ventilation during CPR.[1-3] To address this problem, studies for preventing excessive ventilation have been conducted using simple methods such as a metronome, thoracic impedance, capnography, and tracheal pressure monitoring.[4-8] However, it is difficult to maintain a proper tidal volume (Vt) and ventilation rate with a self-inflating bag resuscitator during CPR. One study on actual CPR showed that use of a self-inflating bag resuscitator is likely to result in excessive ventilation and high airway pressure in practice,[9] whereas using an automatic transport ventilator instead of a self-inflating bag resuscitator shows better outcomes.[10-12]
Despite various efforts, the study of ventilation during CPR has not provided adequate evidence on ventilation rate, Vt, or peak airway pressure (Ppeak). Moreover, when unexpected cardiac arrest occurs in patients, no studies or guidelines direct the use of a mechanical ventilator. We conducted this study to determine whether the use of a mechanical ventilator during CPR is adequate to maintain the ventilation rate, Vt, and Ppeak.
Materials and Methods
1) Experimental protocol and data collection
We conducted this study at a tertiary teaching hospital from March 2013 to May 2013.
One manual self-inflating bag resuscitator (Ambu® Resuscitator Mark IV, Ambu, Ballerup, Denmark), and 1 mechanical ventilator were used in Model 1 (CPR manikin without compression) and Model 2 (CPR manikin with compression).
A CPR manikin (Resusci Anne Skill Reporter™, Laerdal, Stavanger, Norway), which allows the evaluation of the adequacy of CPR, was connected to a flow analyzer by a 7.0 mm endotracheal tube and a 1-way valve (Fig. 1).
With a self-inflating bag resuscitator, we performed ventilation at 10 breaths/min and used the volume-marked bagvalve procedure[13] to control Vt. The mechanical ventilator (MV2500 SU:M3, MEK-ICS CO., Seongnam, Korea) was used under the same conditions for volume-controlled mandatory ventilation: Vt 600 mL, inspiration time (Ti) 1.2 sec, constant flow pattern, ventilation rate 10 breaths/min, and positive end expiratory pressure (PEEP) 3 cmH2O. We set the triggering limit to maximum and divided the pressure limit (Plimit) into 3 subgroups to test Model 2 (Plimit: 40, 50, 60 cmH2O). We used a flow analyzer (Flowanalyser™ PF-300, Imtmedical, Switzerland) to measure Ppeak and Vt in each group. Ventilation was considered adequate when Vt was in the range of 400–600 mL[14-16] and Ppeak was ≤ 50 cmH2O.
Chest compression was performed by 4 emergency medicine residents on the floor, and ventilation was performed by 1 emergency medicine resident; all residents were certified advanced cardiac life support providers. A total of 10 minutes of chest compressions were used in each subgroup, and chest compression depth (5–6 cm) and rate (100/min) were maintained, as verified by a skilled reporter. The ventilation (10 breaths/min) was verified by the flow analyzer. The 4 chest compression performers took 2-minute turns to reduce the effect of performer fatigue.
2) Statistical analysis
We used the Kruskal-Wallis test to compare the continuous variables; each value represented the median value and quartile. We used the χ2 test or Fisher’s exact test to analyze the discrete variables. PASW 18.0 (SPSS Inc., Chicago, IL, USA) was used to compile statistics, and the significance level was p<0.05.
Results
1) Comparison between the ventilation equipment used on the manikin
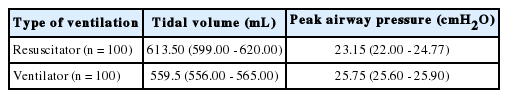
Compliance and resistance were 35 mL/cmH2O and 20 cmH2O/L/sec, respectively, with the manikin prepared as shown in Fig. 1. Ventilation equipment Vt and Ppeak were in an appropriate range (Table 1).
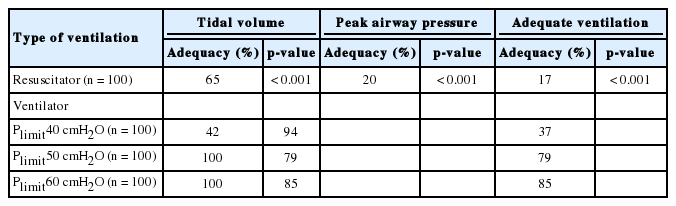
2) Comparison between the ventilation equipment during chest compression (Table 1 and Fig. 2)
Changes of the tidal volume and peak airway pressure in Model 2. Model 2; CPR Manikin with compression, Resuscitator; self-inflating bag resuscitator, ventilator 1; Plimit 40 cmH2O, 2; Plimit 50 cmH2O, 3; Plimit 60 cmH2O, Tidal volume adequacy; Vt 400-600 mL, Peak airway pressure adequacy; Ppeak ≤ 50 cmH2O, Adequate ventilation; Vt 400-600 mL and Ppeak ≤ 50 cmH2O
When a self-inflating bag resuscitator was used during chest compression, an adequate Vt and Ppeak were observed at 17%. When an adequate Vt was maintained, Ppeak over 50 cmH2O was 48%.
A mechanical ventilator with CPR produced the following results: With Plimit set at 40 cmH2O, it was possible to maintain Ppeak at 94% and Vt at 42%; an adequate Vt and Ppeak level was 37%. With Plimit set at 50 cmH2O, it was possible to maintain Ppeak at 79% and Vt at 100%; an adequate Vt and Fig. 1. Closed loop manikin circuit connected to flow analyzer. Ppeak level was 79%. With Plimit set at 60 cmH2O, it was pos sible to maintain Ppeak at 85% and Vt at 100%; an adequate Vt and Ppeak level was 85%.
Discussion
In its 2010 guidelines, the American Heart Association (AHA) suggested that high-quality CPR should maintain a rate of at least 100 compressions/min and a compression depth of at least 2 inches (5 cm) in adults to allow complete chest recoil after each compression, minimize interruption in chest compression, and prevent excessive ventilation. The AHA also advised that CPR should be performed at the rate of 8–10 breaths/min, allowing 400–600 mL of ventilation without interruption of chest compression when an endotracheal tube is inserted.[17] Despite those guidelines on ventilation, proper ventilation has not yet been clearly set. Despite many studies, the effort to determine an optimal Vt and ventilation rate has been unsuccessful.[18,19] Meanwhile, the more hyperventilation occurs during CPR, the more positive pressure is created, leading to increased intrathoracic pressure,[9,20] which could decrease survival rates by reducing venous return, cardiac output, and coronary perfusion pressure.[21-23] Those side effects in hemodynamics tend to be caused by changes in the ventilation rate rather than changes in Vt.[9, 24-27] Therefore, guidelines based on recent studies suggest reduced Vt, compared with the past, and a restricted ventilation rate.
According to a study by Aufderheide et al.,[22] rescuers consistently hyperventilated patients during pre-hospital CPR, and subsequent animal studies showed that mean intrathoracic pressure increased from 7.1±0.7 mmHg/min to 17.5±1.0 mmHg/min when the ventilation rate increased from 12 breaths/min to 30 breaths/min during CPR. To solve this problem, a real-time audiovisual feedback system that maintains the ventilation rate at a certain level has been suggested for use with a self-inflating bag resuscitator. However, although a self-inflating bag resuscitator with an additional device could control the ventilation rate, it might not control Vt. The volume-marked bag-valve procedure, which we used in this study, could solve that problem, but its effectiveness has not yet been proved, and that is beyond the scope of this study. In fact, it is not easy to simultaneously obtain a certain level of Vt and Ppeak with a self-inflating bag resuscitator.
For this reason, we determined whether a mechanical ventilator might be used during CPR to maintain ventilation rate, Vt, and stable intrathoracic pressure. We found that when volume-controlled mandatory ventilation was set at Vt 600 mL, Ti 1.2 sec, constant flow type, ventilation rate 10 breaths/min, PEEP 3 cmH2O, maximum pressure triggering, and Plimit 60 cmH2O, Vt and Ppeak retained relatively high adequacy, as compared with the other subgroups of the mechanical ventilator and the self-inflating bag resuscitator. According to Maertens et al.,[8] the ventilation rate was higher than the setting when a transport ventilator was used because the chest compression caused assisted ventilation from the flow triggering. Therefore, we set the triggering limit to its maximum to prevent assisted ventilation.
In a real situation, very high Ppeak was observed as a result of hyperventilation, suggesting a higher risk of barotrauma. In this context, it is necessary to set an adequate Plimit to prevent barotrauma when proper Vt is guaranteed. In Model 2, the self-inflating bag resuscitator Plimit median value was 53.2 cmH2O (IQR 50.73–58.75), and the mechanical ventilator was 46.3 cmH2O (IQR 42.90–49.20) with a Plimit of 60 cmH2O (Table 3). We suggest that a Plimit of 60 cmH2O is adequate to prevent barotrauma.
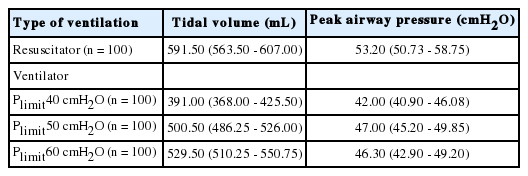
Comparison of median value (IQR) among the ventilation equipment during chest compression in model 2 (CPR Manikin with compression)
The manikin we used showed lower compliance and higher resistance than a normal human being, which might be a limitation to this study. Compliance was lower because the manikin’s artificial lung was stiff, and resistance was higher because the length of the circuit was longer than a human airway. In a human airway, inspiration and expiration occur through the same lumen, whereas we used separated lumens in this study. An adequate mechanical ventilator mode for human CPR needs to be identified in further studies. However, this study showed that the adequacy of Vt and Ppeak using a mechanical ventilator was higher than that using a self-inflating bag resuscitator in CPR. Moreover, it is difficult to maintain Vt and Ppeak during CPR when using a self-inflating bag resuscitator because excessive Vt or insufficient Vt occur often.[2,9] We suggest that a mechanical ventilator set to the proper mode can provide steadier and more stable ventilation than a self-inflating bag resuscitator.
In our manikin model, the mechanical ventilator was superior to the self-inflating bag resuscitator for maintenance of adequate ventilation during chest compression. Using a mechanical ventilator that can maintain adequate Vt and ventilation rate can prevent excessive ventilation. A mechanical ventilator that can maintain Ppeak < 50 cmH2O can also prevent barotrauma.
Although we found differences according to the Plimit,, we conclude that a mechanical ventilator might be used to achieve high quality CPR in patients with endotracheal intubation.
Notes
No potential conflict of interest relevant to this article was reported.