Plasma biomarkers for brain injury in extracorporeal membrane oxygenation
Article information
Abstract
Extracorporeal membrane oxygenation (ECMO) is a life-saving intervention for patients with refractory cardiorespiratory failure. Despite its benefits, ECMO carries a significant risk of neurological complications, including acute brain injury (ABI). Although standardized neuromonitoring and neurological care have been shown to improve early detection of ABI, the inability to perform neuroimaging in a timely manner is a major limitation in the accurate diagnosis of neurological complications. Therefore, blood-based biomarkers capable of detecting ongoing brain injury at the bedside are of great clinical significance. This review aims to provide a concise review of the current literature on plasma biomarkers for ABI in patients on ECMO support.
INTRODUCTION
Over the past 30 years, extracorporeal membrane oxygenation (ECMO) has been increasingly deployed to provide life-saving circulatory support to patients with refractory pulmonary and cardiac pathology [1]. Venoarterial (VA)-ECMO is used as the rescue of refractory cardiac failure and venovenous (VV)-ECMO is used for refractory respiratory failure. Despite its benefits, current literature indicates an overall ECMO survival rate of 29%, with acute brain injury (ABI), including acute ischemic stroke (AIS), intracranial hemorrhage (ICH), and hypoxic-ischemic brain injury, being a leading cause of morbidity and mortality [2]. Further, ABI confers a two- to three-fold increase in mortality risk for patients on ECMO [2-4]. Standardized neuromonitoring protocols improve the detection of ABI and include iterative neurological exams, near-infrared spectroscopy, transcranial doppler, electroencephalograms, and somatosensory evoked potential and neuroimaging studies (Figure 1) [3,4].
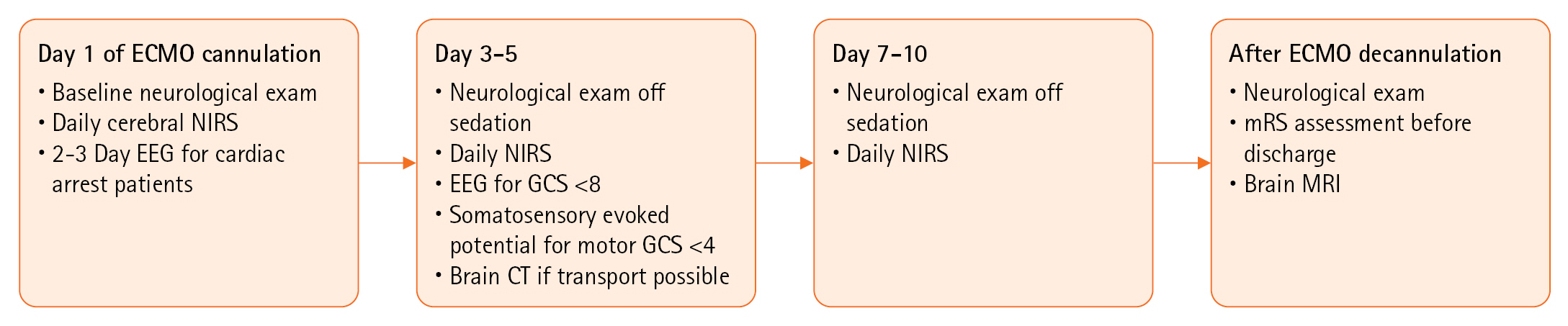
Standardized neuromonitoring protocol. ECMO: extracorporeal membrane oxygenation; NIRS: near-infrared spectroscopy; EEG: electroencephalogram; GCS: Glasgow Coma Scale; CT: computed tomography; mRS: modified Rankin Scale; MRI: magnetic resonance imaging. Adapted and Retrieved from Ong CS, et al. J Thorac Cardiovasc Surg 2023;165:2104-10 [4], to which biomarkers could be supplementary once more studied in ECMO.
However, neuroimaging during ECMO is challenging. Head computed tomography (CT) scans lack sensitivity to detect early and small ischemic events. Moreover, head CT scans are obtained in only 30% of ECMO patients due to the increased risks of transporting patients while cannulated for ECMO [3]. Brain magnetic resonance imaging (MRI) is more sensitive for identifying ischemia but MRI with high-strength magnetic fields (1.5–3T) is incompatible with ECMO [5]. Additionally, most patients receiving ECMO support would not be stable enough to undergo a prolonged imaging study outside of the intensive care unit. To overcome these limitations, the development and validation of accessible plasma biomarkers that are sensitive and specific for ABI are necessary. Consequently, there has been a recent interest in plasma biomarkers for patients on ECMO (Figure 2). The purpose of this review is to concisely consolidate and critically appraise our current understanding of plasma biomarkers and their role in monitoring and prognostication of ABI and their applicability in patients on ECMO support.
BIOMARKERS STUDIED IN ECMO
Biomarkers in VA-ECMO
Neuron-specific enolase
Neuron-specific enolase (NSE) is a glycolytic enzyme prevalent in neurons and neuroendocrine cells [5]. NSE bloodstream levels, which begin to increase several hours after neuronal damage and peak at 48 hours post-injury, are a potential biomarker for brain injury in patients undergoing ECMO [6,7]. Several studies have focused on elucidating the role of NSE in various clinical settings. A prospective multicenter study involving 623 out-of-hospital cardiac arrest (OHCA) survivors revealed a significant difference in median NSE levels between patients with non-shockable and shockable rhythms (104.6 ng/ml [range, 40.6–228.4] vs. 25.9 ng/ml [range, 16.7–53.4], P<0.001) [6]. In a retrospective multicenter study on 70 traumatic brain injury (TBI) patients, higher NSE concentrations corresponded with increased injury severity and adverse neurological outcomes [8].
The utility of NSE as a biomarker for patients on ECMO is still under investigation. A prospective study involving 80 pediatric ECMO patients indicated elevated NSE levels in those developing neurological complications [9]. Specifically, elevated plasma concentrations of NSE, with a cutoff of 62.0 ng/ml, were associated with increased odds (adjusted odds ratio, 2.89) of unfavorable outcomes, measured by Pediatric Cerebral Performance Category, at hospital discharge [9]. These findings are consistent with another retrospective single-center study of 30 adults in a VA-ECMO cohort, which showed that NSE peak values above a cutoff of >100 μg/L had a sensitivity and specificity for mortality of 0.53 and 0.82, respectively [10].
However, it’s important to highlight that the specificity of NSE in ECMO patients may be compromised by erythrocyte hemolysis, a frequent occurrence in ECMO, which can lead to elevated NSE levels, complicating its reliability in detecting ABI and predicting neurological outcomes [11]. Future prospective multicenter research is necessary to understand specific NSE thresholds and dynamic kinetics in relation to ABI in ECMO patients.
Glial fibrillary acidic protein
Glial fibrillary acidic protein (GFAP) is a specific type of intermediate filament protein, involved in the structural integrity and functioning of astrocytes within the central nervous system (CNS). The unique localization of GFAP to astrocytes in the brain emphasizes its potential as a sensitive biomarker for detecting brain injuries. Astrocytes undergo astrogliosis—a reactive process involving cellular proliferation and increased GFAP production—indicating neuronal damage [12]. GFAP is elevated within about 2 hours following injuries such as AIS [13-15], cardiac arrest [16,17], and TBI [18-22], peaking at 48–72 hours [23], and thus may be useful for monitoring both neurologic and non-neurologic complications in ECMO.
In a pediatric single center VA-ECMO cohort (n=80), GFAP levels were measured by immunoassay at 6 and 12 hours, and then every 24 hours after cannulation [9]. GFAP levels were found to be significantly elevated in children on ECMO who experienced ABI compared with children who did not, with a median of 5.9 versus 0.09 ng/ml (P=0.04) [9]. Additionally, higher GFAP levels were found in non-survivors compared to survivors. GFAP levels over 0.436 ng/ml were associated with increased odds ratio (OR) of brain injury (OR, 11.5; 95% confidence interval [CI], 1.3–98.3) and mortality (OR, 13.6; 95% CI, 1.7–108.5) [9]. However, this study was limited by the small sample size and the difficulty of accurately diagnosing ABI. A pilot single-center study by Kapoor et al. [24] (n=20) corroborated these findings in adults on VA-ECMO support, with median plasma GFAP levels noted to be significantly higher for patients who developed ABI vs. without (5.17 ng/ml vs. 0.16 ng/ml, P=0.047). The findings from these pilot studies warrant further research in larger cohorts to validate and define their clinical applications.
Tau
Tau proteins are microtubule-associated proteins involved in stabilizing the cytoskeleton, particularly in unmyelinated axons of the CNS [25]. While they are most abundant in neurons, they are also found in astrocytes and oligodendrocytes [25]. Like neurofilament light chain (NfL), tau protein released into the cerebrospinal fluid (CSF) can potentially be used as a biomarker indicating axonal damage. Tau has been most heavily studied in its misfolded aggregate form in Alzheimer disease and other forms of dementia, such as chronic traumatic encephalopathy in athletes playing contact sports [26,27].
Elevated tau has shown promise as a marker for adverse clinical outcomes following TBI. In a pilot, single-center prospective study of 16 patients, microdialysis catheter measurement of tau from the brain extracellular space following TBI correlated with a lower Glasgow Coma Scale (GCS) score 6 months after injury (r=–0.6, P=0.018) [28]. Additionally, tau levels were highest when catheters were near the area of the contusion, verifying the use of tau as a marker of axonal damage [26]. These conclusions were strengthened by another single-center prospective study (n=50), which showed that CSF tau levels correlated with AIS severity (P<0.05). In this study, higher CSF tau levels were also correlated with a worse outcome defined by the modified Rankin Scale (mRS) score at 12 months [29]. In an international multicenter prospective study (n=689), increased serum tau soon after OHCA was predictive of poor neurological function at 6 months, as measured by the Cerebral Performance Categories (CPC) scale. At 48 hours following cardiac arrest, the median tau levels were 49.5 ng/L in the poor outcome group, and only 1.2 ng/L in the favorable outcome group (P<0.0001) [30]. Tau levels may be useful for more extended neuromonitoring, as while elevations begin as early as 6 hours post-injury, peak elevations are as late as 6 days following injury [31].
Despite the promising results of tau protein predicting outcomes in neurological diseases, evidence is very limited in ECMO patients. A pilot single-center prospective observational cohort study by Kapoor et al. [24] (n=20) reported a higher trend in plasma tau values for patients with ABI vs without ABI on VA-ECMO (1.87 ng/ml vs. 0.44 ng/ml, P=0.62). This study was limited by its sample size and was unable to reach appropriate power for statistical significance. While tau shows promise as a biomarker after TBI and cardiac arrest, its utility for patients on ECMO needs to be further explored.
Neurofilament light chain
Neurofilaments are intermediate filaments that help comprise the cytoskeleton of neurons. The triplet consists of three subunits, including NfL, neurofilament medium chain, and neurofilament heavy chain [32]. NfL is a neuron-specific protein residing in the cytoplasm of large, myelinated axons [32]. NfL has been studied as a potential biomarker, as its release into the CSF as early as several hours after injury can indicate neuronal death and more specifically axonal damage [33,34]. To date, NfL has been most thoroughly studied in multiple sclerosis, TBI, and cardiac arrest, and its application in other neurologic disorders has recently been explored including stroke, lysosomal storage disorders, amyotrophic lateral sclerosis, and frontotemporal dementia.
NfL has shown promise as a marker for outcome prediction in patients with OHCA. An international, multi-center (29 sites) prospective study of 782 adults demonstrated that serum NfL levels measured 1–3 days after OHCA were sensitive and specific for worse neurological outcomes by CPC score at 6 months, and this prognostic performance exceeded that of other biomarkers and standardized neuromonitoring (CT, somatosensory evoked potentials, electroencephalogram, and neurological exam) [35]. A multicenter prospective study of 248 adults validated these findings and found that median serum NfL concentrations 48 hours after OHCA was 0.019 ng/ml in patients with good neurological outcomes by CPC score and 2.343 ng/ml in those with poor neurological outcomes (P<0.001) [36]. In a retrospective multicenter observational study (n=428) looking at CPC outcomes for both OHCA and in-hospital cardiac arrest (IHCA), NfL at 12 hours was superior to NSE at 24 hours (area under the curve [AUC]: 0.93 vs. 0.83 for OHCA and AUC: 0.87 vs 0.71 for IHCA) [37]. NfL at 48 hours was superior to NSE at 48 hours (AUC: 0.97 vs. 0.90 for OHCA, and AUC: 0.90 vs. 0.77 for IHCA) [37].
A pilot prospective single-center cohort study (n=20) reported a significant difference in NfL values for patients with ABI vs without ABI on VA-ECMO (13.6 ng/ml vs. 3.42 ng/ml, P=0.007), which may be better than GFAP and tau protein in predicting ABI and neurological outcomes in ECMO patients [24]. In summary, serum NfL appears to be the most promising biomarker with consistent demonstration of high sensitivity and specificity across various forms of brain injury. Further studies to determine accurate cutoffs are warranted for ECMO patients.
Biomarker Applications Studied in VV-ECMO
MicroRNA
MicroRNAs (miRNAs) are a class of single-stranded, non-coding RNA fragments involved in regulating gene expression in many pathways [38]. While currently difficult to implement miRNA in a critical care setting due to the cost and time needed to determine miRNA sequencing signatures, a prospective study in 11 adult VV-ECMO patients with severe acute respiratory distress syndrome (ARDS) found that serum levels of 13 miRNAs in were markedly upregulated (vs. those with less severe disease) as measured by Sequential Organ Failure Assessment (SOFA), respiratory ECMO survival prediction score, and Simplified Acute Physiology Score (SAPS) II [38]. miRNAs increased in severe ARDS were found to be members of tissue remodeling, blood coagulation, and immune regulation pathways, in line with processes found to contribute to further injury in ARDS patients [38]. While not specifically studying neurological outcomes, as miRNA sequencing becomes more available and cost-effective, similar miRNA upregulation signatures could be identified specifically for neurological injury. The breadth of available miRNAs means that biomarkers could be unique according to tissue type, and even to processes such as ischemic and hemorrhagic stroke.
Biomarker Applications Studied in VA-ECMO and VV-ECMO
Inflammatory cytokines
Inflammatory cytokines such as interleukin (IL)-6, IL-1, IL-8, and tumor necrosis factor (TNF) -α are small, secreted molecules controlling cell-cell interaction in the setting of inflammation regulation [39]. While it has been well-established that inflammatory cytokines rise throughout the duration of ECMO therapy [40], few studies have focused on inflammatory cytokines as predictors of neurological injury in the setting of ECMO. One prospective pediatric study of 99 patients undergoing both VA-ECMO and VV-ECMO found significant elevations in inflammatory markers including interferon gamma (IFN-γ), IL-6, IL-1β, and TNF-α in children with abnormal head imaging (diffuse hypoxic injury, ICH, or ischemic stroke on ultrasound, CT or MRI) compared to children with normal head imaging. Additionally, IL-6 concentration was significantly elevated in children who did not survive their hospitalization compared to children who did, both on ECMO day 1 (median, 98.5 vs. 23.1 pg/ml) and at peak (median, 102.8 vs. 32.6 pg/ml) [41].
A prospective observational cohort study (n=266) on inflammatory cytokines in adults undergoing VV-ECMO found that higher inflammatory cytokines during ECMO were associated with a lower chance of survival, suggesting that increased inflammation during ECMO may be a potential prognostic biomarker [42]. This study also showed that levels of inflammatory cytokines including IL-6, IL-8, and TNF-α fell after discontinuing mechanical ventilation and switching to ECMO [42]. While mechanisms were not fully explored, patients undergoing mechanical ventilation with positive end-expiratory pressure (PEEP) ≥15 cm H2O and/or driving pressures ≥ 19 cm H2O prior to ECMO had higher inflammatory cytokine levels than those who had required lower PEEP and driving pressures [42]. Oncostatin M (OSM) is an inflammatory cytokine in the IL-6 family that is expressed in neurons, astrocytes, glia, and immune cells infiltrating the CNS, but also in non-neural tissue, such as lung and liver [43]. However, the role of OSM in ABI is controversial, with conflicting evidence. A prospective study of 29 VV-ECMO patients found that pre-decannulation OSM was elevated in VV-ECMO patients who did not survive compared to those who did (Mann-Whitney U-test: P=0.04) [43]. However, prior murine models have demonstrated that increased OSM expression is associated with improved neurological recovery following AIS, in contrast to the VV-ECMO study [44]. While studies of OSM after ABI have been contradictory, prior studies in lung injury have shown that OSM is released by infiltrating immune cells, with increased OSM serving as a marker of tissue injury [45]. However, given that OSM is not specific to neurological injury, and prior results have been conflicting, OSM may not be as useful compared to other brain-specific biomarkers that are discussed in this review.
Overall, inflammatory cytokines as an umbrella category are of variable utility as predictors of neurological injury in the setting of ECMO. Inflammatory cytokines such as IFN-γ, IL-6, IL-1β, and TNF-α have shown utility as an indicator of neurological complications in the pediatric ECMO population and as predictors of mortality in the adult population and require further study to establish reference ranges in the setting of various types of neurological injury. Conversely, OSM has shown conflicting results in various studies and lacks neurological specificity, and thus its utility in indicating neurological injury during ECMO may be limited.
POTENTIAL BRAIN-SPECIFIC BIOMARKERS FOR ECMO PATIENTS
Mitochondrial DNA
Mitochondrial DNA (mtDNA), sometimes referred to as circulating free mtDNA, fragments are released when cells are affected by mechanical or biological injury (as in hypoxia or inflammation) [46]. Physiologically, mtDNA appears to potentiate the immune response via toll-like receptors [46-48]. mtDNA levels have previously shown utility in predicting disease severity and mortality in critically ill patients with sepsis and acute lung injury [49,50].
In the setting of mechanical circulatory support, investigations into the role of mtDNA are limited. In a prospective study of 962 adult patients with post-cardiopulmonary bypass, mtDNA levels positively correlated with N-terminal prohormone of brain natriuretic peptide (NT-proBNP) levels and Acute Physiology and Chronic Health Evaluation (APACHE) II score, an estimate of intensive care unit mortality risk [51]. In an ex vivo ECMO model that circulated heparinized human blood for 6 hours at differing flow rates, mtDNA was associated with loss in platelet function as measured by thrombelastography platelet mapping and collagen agonist stimulated responses [52]. mtDNA levels may have utility in predicting coagulation complications in ECMO patients, particularly in patients with ischemic and hemorrhagic strokes. In a single-center prospective study (n=100), mtDNA levels were significantly higher in patients with AIS compared to controls (P<0.05), positively correlated with clinical severity of stroke as determined by the National Institute of Health Stroke Scale, and that plasma mtDNA levels decreased with time after stroke (follow-up for up to 30 days, P<0.001) [53].
In summary, mtDNA is a promising biomarker specifically for patients with coagulation complications in ECMO. Further research specifically in these cohorts across centers is necessary to validate these findings and determine accurate cutoffs.
Cell-Free DNA
Cell-free DNA (cfDNA) is a novel biomarker consisting of double-stranded DNA fragments released into the bloodstream under conditions of tissue stress resulting in cellular apoptosis or necrosis [54]. While cfDNA has been studied primarily in current literature in its application in liquid biopsy for oncological diagnosis and management, there has been a recent uptick in understanding the role that cfDNA may play in acute neurological conditions. In a prospective study of 54 patients with AIS, cfDNA was elevated in blood samples collected within 48 hours of AIS treated with IV thrombolysis compared to healthy controls [55]. Further, cfDNA levels on admission were able to discriminate between AIS and stroke mimics. An analysis of the plasma beta-globin gene allowed discrimination between AIS and ICH [55]. Similarly, in a prospective study of 54 Indian patients with AIS, cfDNA level was shown to correlate with poor neurological outcomes (measured by mRS score) at 3 months [56]. Additionally, in a prospective study of 60 patients admitted after acute ICH, higher plasma nuclear DNA levels at presentation correlated with poorer GCS scores [57]. Plasma cfDNA levels have also been shown to be predictive not only of worse functional outcomes, but also of stroke size at onset. In a prospective study of 88 patients presenting to the emergency department with stroke-like symptoms, plasma cfDNA taken within 3 hours of symptom onset correlated with ICH volume as measured by CT [58]. Although there are no studies using cfDNA in ECMO patients, given the utility of cfDNA in predicting stroke volume and severity, plasma cfDNA levels may be useful as an early indicator of possible stroke in ECMO patients.
Lipidomics and Metabolomics
Lipidomics and metabolomics offer a promising new avenue for markers of TBI, due to the increased permeability of the blood brain barrier (BBB) to lipids compared to proteins [59]. Cellular injury occurring after TBI carries with it a plethora of metabolic effects, resulting in derangements in processes such as oxidative phosphorylation and activation of phospholipase C and D, thereby triggering downstream signaling cascades. When the rat serum lipidome was analyzed 3 and 7 days after a controlled cortical TBI, lipidome panels achieved 85% accuracy at differentiating rats having undergone TBI from the control rats. Amongst lipids analyzed, polyunsaturated fatty acids (PUFAs), specifically free fatty acids, increased after TBI, while oxidized fatty acids decreased. Additionally, PUFA-esterified diacylglycerols increased, due to phospholipase signaling [59]. In further work by the same group, sensitivity of the lipidome panel exceeded 90% for lipidomic changes occurring within 24 hours following TBI. Sphingolipids, specifically sphingomyelins (SM), were increased as early as 4 hours following the injury, due to increased cell death. Additionally, ceramides were found to be increased, due to increased necroptosis [60].
In a metabolomic cohort study of 716 patients with TBI, carbohydrates derivatives including myoinositol, found in glial cells, were found to be elevated following TBI, which was postulated to be due to disruption of the BBB. Conversely, higher levels of phospholipids, including phosphatidylcholines, lysophosphatidylcholines, and SM, were correlated with decreased severity of TBI as well as improved functional outcomes [61]. Higher circulating levels of lysophospholipids were also found to be associated with improved outcomes in patients with mid TBI [62]. These results highlight the complex effects of circulating phospholipids and significant differences in the systemic response to ABI in humans compared with rodent models. Further research is needed to better characterize the functional consequences of altered lipid levels after ABI before they can be used effectively as clinical biomarkers.
While lipidomic and metabolomic changes have not yet been correlated to neurological complications of ECMO, the stability of lipids and their easier passage across the BBB make them promising candidates as biomarkers of ABI. Given the few numbers of studies, more work is needed in human subjects to characterize both lipidome and metabolome derangements, as well as their pathophysiology, prior to application in patients at risk for ABI including those on ECMO support. To fully assess the risk of ABI in patients on ECMO support, the integration of multi-omic data including metabolomics, proteomics, and genomics is recommended (Table 1).
CONCLUSIONS
Plasma biomarkers hold significant promise for the early detection and monitoring of ABI in ECMO patients. While research in other applications has been growing, there is limited data on biomarker applications in ECMO patients. The nascent stage of this research field, particularly in the context of ECMO, necessitates a comprehensive exploration and validation of these biomarkers. While some biomarkers like GFAP and NfL have shown promise, a vast array of other potential candidates remains unexplored in ECMO patients. Further research is needed to validate their clinical utility and to establish reliable biomarker panels tailored to specific patient populations and brain injury types. Future studies should focus on larger, well-defined ECMO cohorts (ECMO indications and cannulation strategy), understanding the dynamic kinetics and threshold for ECMO-associated ABI, and adopt standardized methodologies. By advancing our understanding of the complex interactions between brain injury, ECMO, and plasma biomarkers, clinicians will be better equipped to identify patients at risk, monitor their progress, and improve patient outcomes.
HIGHLIGHTS
▪ A comprehensive evaluation and critical appraisal of a range of biomarkers including neuron-specific enolase, glial fibrillary acidic protein (GFAP), inflammatory cytokines, microRNA, tau protein, neurofilament light chain (NfL), mitochondrial DNA, cell-free DNA, lipidomics, and metabolomics have been outlined, revealing their potential in predicting acute brain injury and neurological outcomes in extracorporeal membrane oxygenation (ECMO) patients.
▪ GFAP and NfL are biomarkers that offer the most promise for clinical utility.
▪ There is a need for further multicenter research to develop standard thresholds to optimize the application of these biomarkers in patients on ECMO support.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
SMC was supported by National Heart, Lung, and Blood Institute (1K23HL157610). AMG was supported by National Institute of Neurological Disorders and Stroke (5K23NS121628).
ACKNOWLEDGMENTS
None.
AUTHOR CONTRIBUTIONS
Conceptualization: SK, SMC. Funding acquisition: SMC. Writing–original draft: all authors. Writing–review & editing: all authors.


