Abstract
-
Background
- Killip-Kimball classification has been used for estimating death risk in patients suffering acute myocardial infarction (AMI). Killip-Kimball stage IV corresponds to cardiogenic shock. However, the Society for Cardiovascular Angiography and Interventions (SCAI) classification provides a more precise tool to classify patients according to shock severity. The aim of this study was to apply this classification to a cohort of Killip IV patients and to analyze the differences in death risk estimation between the two classifications.
-
Methods
- A single-center retrospective cohort study of 100 consecutive patients hospitalized for “Killip IV AMI” between 2016 and 2023 was performed to reclassify patients according to SCAI stage.
-
Results
- Distribution of patients according to SCAI stages was B=4%, C=53%, D=27%, E=16%. Thirty-day mortality increased progressively according to these stages (B=0%, C=11.88%, D=55.56%, E=87.50%; P<0.001). The exclusive use of Killip IV stage overestimated death risk compared to SCAI C (35% vs. 11.88%, P=0.002) and underestimated it compared to SCAI D and E stages (35% vs. 55.56% and 87.50%, P=0.03 and P<0.001, respectively). Age >69 years, creatinine >1.15 mg/dl and advanced SCAI stages (SCAI D and E) were independent predictors of 30-day mortality. Mechanical circulatory support use showed an almost significant benefit in advanced SCAI stages (D and E hazard ratio, 0.45; 95% confidence interval, 0.19–1.06; P=0.058).
-
Conclusions
- SCAI classification showed superior death risk estimation compared to Killip IV. Age, creatinine levels and advanced SCAI stages were independent predictors of 30-day mortality. Mechanical circulatory support could play a beneficial role in advanced SCAI stages.
-
Keywords: cardiogenic shock; Killip-Kimball; mechanical circulatory support; Society for Cardiovascular Angiography and Interventions classification
INTRODUCTION
Cardiogenic shock (CS) is one of the deadliest critical cardiac conditions, with a 30-day death rate of 30%–50% [1-4]. CS is mainly caused by acute myocardial infarction (AMI) and occurs in about 5%–10% of patients suffering from AMI [1]. The Killip-Kimball classification has been broadly used to determine the clinical situation and to estimate prognosis [5]. Patients who develop cardiogenic shock secondary to acute myocardial infarction cardiogenic shock (AMICS) have stage IV of this classification. However, the cardiogenic shock spectrum is wide and implies different prognoses along it. The Society for Cardiovascular Angiography and Interventions (SCAI) classification was first published in 2019, defining five stages of cardiogenic shock according to severity. Stage “A” stands for “At risk” and involves a patient who potentially could develop cardiogenic shock (e.g., anterior ST-elevation myocardial infarction with left ventricular dysfunction) but is not currently experiencing signs or symptoms. Stage “B” stands for “Beginning” and involves a patient who is decompensated (tachycardia and hypotension without hypoperfusion). Stage “C” stands for “Classic” and refers to a patient that meets the classic cardiogenic shock criteria, showing hypoperfusion signs and requiring vasoactive support or even mechanical circulatory support (MCS) to achieve stabilization. Stage “D” stands for “deteriorating” and involves a patient who could not be stabilized with initial therapies and maintains a hypoperfusion status and requires additional measures to reverse the condition (e.g., additional drugs or MCS). Finally, stage “E” stands for “Extremis” and involves a patient in deep shock, frequently in refractory cardiac arrest or supported by several MCS devices and drugs [6]. This classification was updated in 2022 to include some modifications in the cut-offs used to define the stages (e.g., lactate, hemodynamic parameters) [7]. An illustrative chart with complete criteria for SCAI classification is provided in Supplementary Figure 1.
Despite several studies validating the use of SCAI classification in patients with CS due to different causes, no prior studies have evaluated the difference in mortality estimation between the Killip IV classification and the different SCAI stages in an AMICS population [8-10].
MATERIALS AND METHODS
We retrospectively analyzed the last 100 patients who experienced cardiogenic shock admitted to the acute cardiac care unit of our hospital with a Killip IV AMI diagnosis between January 2016 and October 2023. Our center is a tertiary hospital with a 24-hour available cath-lab and cardiac surgery team but with no long-term assist devices or heart transplantation program. No extracorporeal cardiopulmonary resuscitation (e-CPR) program was operative during the study period.
Cardiogenic shock was defined as systolic blood pressure ≤90 mm Hg maintained for at least 30 minutes and a cardiac index ≤2.2 L/min/m2 or need for vasoactive drugs or mechanical support to achieve systolic blood pressure or cardiac index above the cut-off level, according to the definition provided by the National Cardiovascular Data Registry [11]. Exclusion criteria included all types of non-AMI-derived cardiogenic shock and missing data that prevented reclassification in SCAI stages.
Patient demographics and comorbidities; angiographic, echocardiographic, and analytic parameters (peak values during hospitalization); systolic blood pressure at admission; vasoactive index score (VIS); orotracheal intubation or mechanical ventilation; mechanical support; and type of mechanical support were included in this study. Temporal trends associated with mechanical support and its influence on patient prognosis were explored (two time periods were compared: before and after year 2020).
We retrospectively classified these patients in different SCAI stages according to the criteria proposed by the 2022 SCAI SHOCK Stage Classification Expert Consensus Update [7]. The VIS calculation was performed according to the formulae indicated in Belletti et al. [12] (Supplementary Table 1).
The study protocol was approved by the Ethics Committee of Badajoz University Hospital Complex (No. CEI 032/23) and was conducted in accordance with the Declaration of Helsinki. Due to the retrospective character of the study, informed consent waiver was authorized by the local ethics committee.
Statistical Analysis
Categorical variables are presented as frequencies (percentages). Normal distribution was explored using the Shapiro-Wilk test. Because most continuous variables did not follow a normal distribution, they are presented as medians and interquartile ranges (IQRs) for uniformity. Differences in categorical variables among SCAI stages were analyzed using the Fischer exact test. The Mann-Whitney U-test for non-normally distributed variables was used to assess differences. Differences in continuous variables among SCAI stages were explored via the Kruskal-Wallis test. Thirty-day survival was analyzed using the Kaplan-Meier method, and comparisons among groups were explored using the log-rank test. Hazard ratio (HR) and 95% confidence interval (CI) values for 30-day mortality were explored using univariate Cox regression models. Cut-off points for continuous variables for inclusion in the model were determined using the Liu index. Variables that showed a P-value <0.1 were introduced in a multiple Cox regression model to explore significant 30-day mortality predictors. A two-tailed P-value <0.05 was considered statistically significant.
RESULTS
Study Population
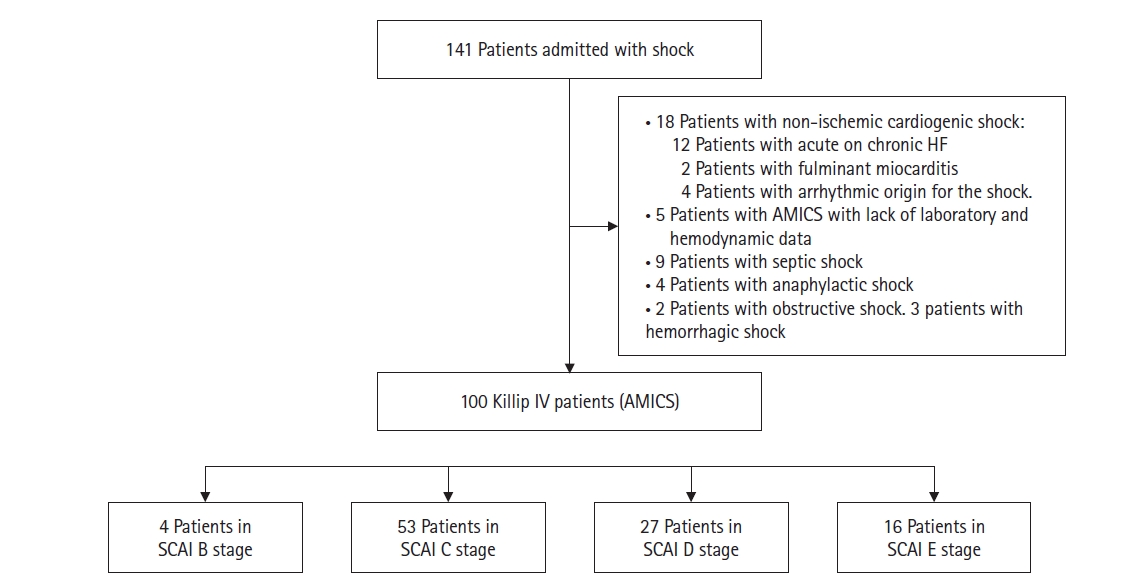
The median patient age was 66 years (IQR, 54–77 years), and 68% of patients were male (Table 1). Upon admission, 87% of patients presented with ST-elevation myocardial infarction, and 86.4% of these patients underwent percutaneous coronary intervention as a first attempt at revascularization, while 13.6% received fibrinolysis. Of these, 91.67% were submitted for rescue PCI. Median systolic blood pressure at admission was 80.0 mm Hg (IQR, 70.0–90.0 mm Hg). Median lactate level was 3.5 mmol/L (IQR, 1.93–6.49 mmol/L). Median creatinine value was 1.33 mg/dl (IQR, 0.94–2 mg/dl). Median aspartate aminotransferase (AST) was 331.5 IU (IQR, 114–557 IU). Median VIS was 20 (IQR, 10–55). Additionally, 60% of patients required orotracheal intubation and invasive mechanical ventilation with a median ventilation time of 48 hours (IQR, 24–96 hours). Median left ventricle ejection fraction (LVEF) was 30% (IQR, 20%–41%). MCS was used in 20% of patients. Use of MCS increased greatly when comparing 2016–2020 to 2020–2023 (12.16 vs. 42.31%, P=0.001). Distribution of patients according to SCAI stage was B=4%, C=53%, D=27%, and E=16% (Figure 1).
Analysis of 30-Day Mortality
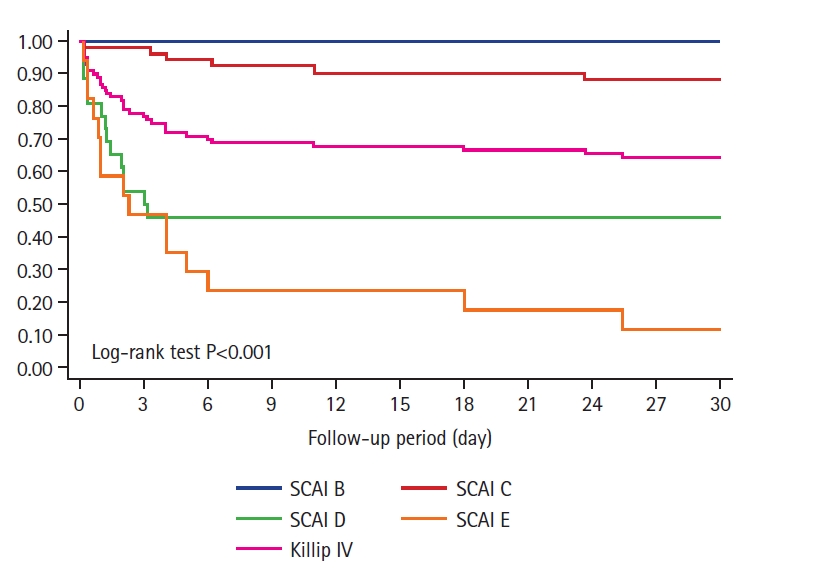
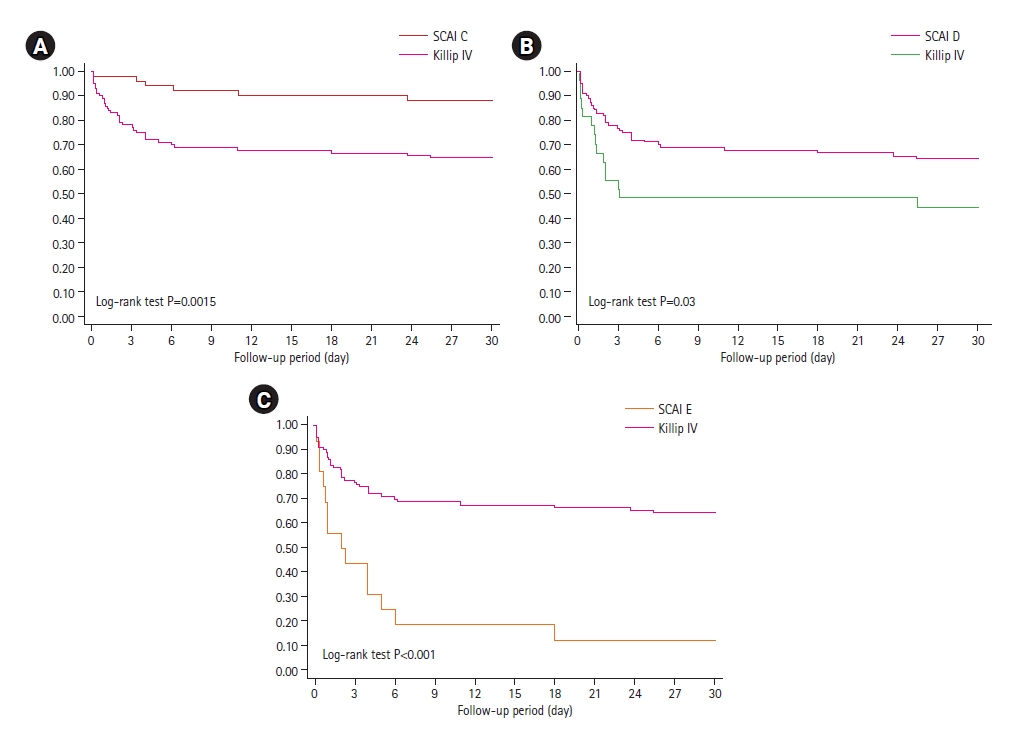
The 30-day death rate was 35% when patients were classified only as Killip IV AMI. As expected, 30-day mortality increased progressively according to SCAI stage (B=0%, C=11.88%, D=55.56%, E=87.50%; log-rank test P<0.001) (Figure 2). Subgroup analysis comparing mortality between Killip IV and established shock SCAI stages (C, D and E) showed significant differences, indicating that Killip IV classification overestimated risk mortality in SCAI C patients (35% vs. 11.88%, log-rank test P=0.002) and underestimated risk mortality in SCAI D and E (35% vs. 55.56% and 87.50%, respectively; log-rank test P=0.03 and P<0.001, respectively) (Figure 3).
Cut-off points for continuous variables were determined using the Liu index as follows: age >69 years, VIS score >20, arterial lactate >3.5 mmol/L,, creatinine >1.15 mg/dl, AST >200 IU/L, and LVEF <20%. Univariate Cox regression showed that all variables had a significant or near significant association with 30-day mortality, advanced SCAI stage (D and E), and previous history of diabetes mellitus. Older age (over 69 years: HR, 2.34; 95% CI, 1.15–4.86; P=0.019), slightly elevated creatinine (creatinine >1.15 mg/dl: HR, 11.52; 95% CI, 1.43–92.77; P=0.022), and advanced SCAI stage (SCAI D: HR, 3.29; 95% CI, 1.20–9.01; P=0.020 and SCAI E: HR, 6.21; 95% CI, 2.28–16.88; P<0.001) were significant predictors of 30-day mortality (Table 2).
Impact of MCS
No significant global benefit was observed from MCS use (P=0.92). However, when we analyzed the impact of MCS in patients with advanced SCAI stages (D and E), a nearly significant benefit was observed (HR, 0.45; 95% CI, 0.19–1.06; log-rank test P=0.058) (Figure 4). This trend was not seen in the other stages.
Patients with MCS presented with lower LVEF (25.63 vs. 33.36%, P=0.023), worse liver function (AST: 857.2 vs. 400.4 IU, P= 0.012), and a nearly significantly worse kidney function (creatinine levels: 2.43 vs. 1.75 mg/dl, P=0.061). Patients who were assisted with MCS also needed more support with vasoactive drugs and higher doses (VIS score: 108.5 vs. 31.56, P<0.001). As SCAI classification stage increased, MCS use increased (0% for SCAI B, 11.32% for SCAI C, 30.77% for SCAI D, and 35.29% for SCAI E; P=0.048). No significant differences in age were found among the SCAI stages, although patients that were assisted with MCS tended to be younger than patients who were not assisted (61.35 vs. 66.99 years, P=0.099).
DISCUSSION
It is established that SCAI classification improves the ability to estimate death risk in cardiogenic shock patients and can be a useful tool to titrate patient’s therapeutic needs [8,9]. In this cohort of 100 patients who developed AMICS, classifying patients only as Killip IV led to an overestimation of mortality compared to SCAI C stage (35% vs. 11.88%, P=0.002) and an underestimation when compared to SCAI D and E stages (35% vs. 55.56% and 87.50% respectively, P=0.03 and P<0.001, respectively). These findings should encourage physicians to use SCAI classification in AMICS patients as the reference prognosis stratification tool and to abandon the outdated solitary concept of Killip IV AMI in these highly complex patients. In addition, we showed that advanced SCAI stages (D and E) were strong predictors of 30-day mortality, which was consistent with several previous findings in which mortality increased with shock severity according to SCAI classification [9,10,13,14].
Distribution of patients according to SCAI stage was similar to the observed in Jentzer et al. [15], except that this work had a larger number of SCAI B patients, in contrast to the predominant SCAI C stage observed in our study. Similarity in number of patients in stages D and E was noted with the 2020 study from Schrage et al. [9]; and the summary of the SCAI A, B, and C patients of that study is very similar to that of our SCAI C patients. These differences could be explained by lack of consideration of SCAI A or most SCAI B patients as Killip IV. The distribution observed in Hanson et al. was also similar to ours [10].
Use of MCS varies widely. A study by Schrage et al. [16] showed 13% of MCS use in a large cohort of 441,696 patients with cardiogenic shock treated in German hospitals between 2005 and 2017. The use of MCS was higher in the AMICS cohort, raising up to 20.15%. Intra-aortic balloon pump (IABP) was the most frequently used device (16.19%), followed by veno-arterial extracorporeal membrane oxygenation (VA-ECMO; 2.31%) and percutaneous left ventricular assist device (pLVAD) (1.65%). This is similar to the MCS use observed in our study [16]. Kim et al. [17] also reported 23% of MCS use. In a recent study from Berg et al. [18], a cohort of patients without invasive hemodynamic assessment in the first 24 hours of admission showed a MCS distribution similar to ours (IABP, 17.6%; Impella, 5.5%; ECMO, 4.2%). However, other studies have found higher MCS use. For example, Jentzer et al. [15] reported 43.5% MCS use in their two-center study, which nearly matches the 42.31% MCS use found in our work for the 2020–2023 period. This increase in MCS use was probably related to the introduction of pLVAD and ECMO devices in our center in 2020. Use of MCS increased according to shock severity, and ECMO and pLVAD were the most used devices in SCAI E stage. We observed a huge increase in MCS use in this stage when comparing the two study periods (10% vs. 71.43%, P=0.035). IABP was the most frequently used device in C and D stages, very similar to percentages reported in Jentzer et al. [14]. No global benefit was observed from MCS, although we found a near significant reduction in mortality in SCAI D and E patients assisted with MCS, which is encouraging given the lack of data showing a clear beneficial effect derived from their use. A larger sample may have yielded a significant result. On the other hand, our center does not have a heart transplantation program or a long-term assist devices program, as our hospital is not a reference center but a referring hospital, and the volume of patients that would reap a potential benefit from short-term therapies is likely lower than that observed in other national reference hospitals with those programs. This may be a main reason why, along with high mortality rate, the length of stay for SCAI E patients seems considerably short in our cohort, because these patients are referred to national referral hospitals as soon as they are stabilized and there is no sign of early cardiac recovery. The absence of an operative extracorporeal cardiopulmonary resuscitation program in our hospital probably influenced the less frequent use of ECMO in SCAI E patients compared with other studies.
Our study is consistent with previous evidence that identified age and kidney injury as significant predictors of short-term mortality in CS patients [19,20]. The relationship between age and shock severity (according to SCAI stage) has also been explored along with its association with death risk in patients with CS [15]. Age did not show a significant association with worse kidney or liver function, higher lactate levels, or VIS score or SCAI stage in our study (all P>0.05). Thus, other age-related factors such as frailty, reduced biological reserve, or delirium should be considered as possible contributors to worse prognosis in elders [21]. Renal function deterioration has been described as a short-term mortality predictor in CS [22,23]. In a sub-study of the IABP-Shock II-trial, which explored novel renal function biomarkers in AMICs, creatinine level >1.32 mg/dl was the only significant predictor of short-term death in AMICS [24]. This value is similar to the cut-off point obtained in our study. These relatively low numbers could indicate a key role of renal impairment in such patients, even in early stages of deterioration. The recently published work by Zweck et al. [25] showed that patients in cardiogenic shock who developed a cardiorenal profile had a higher mortality rate than those with a non-congested profile but a lower rate than those with a cardiometabolic profile.
Our work has some limitations. First, this is a retrospective observational study, so no definitive causalities should be extracted from it. Second, this is a single-center study with a small sample. However, our findings are consistent with previous evidence and provide some new encouraging data for SCAI classification and MCS use in severely ill patients in cardiogenic shock. Future studies with higher-class evidence and larger samples are needed to confirm our findings. Finally, the characteristics of our hospital—a tertiary hospital with no heart transplantation program, long-term assist devices, or an operative e-CPR program during the study period—probably limit extrapolation of our findings to other centers with similar features. Larger reference centers would include patients with different SCAI stages and a higher or at least different proportion of patients assisted with MCS.
KEY MESSAGES
▪ The Society for Cardiovascular Angiography and Interventions (SCAI) classification provides more precise information about shock severity and showed better mortality estimation than Killip-Kimball (stage IV) classification.
▪ Older age, renal function impairment and advanced SCAI stages (D and E) are significant predictors of 30-day mortality in cardiogenic shock secondary to myocardial infarction.
▪ Use of mechanical circulatory support could help to improve the prognosis of patients with advanced SCAI stages.
NOTES
-
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
FUNDING
None.
-
AUTHOR CONTRIBUTIONS
Conceptualization: JPC, CAAL, RNR, JMNA, JRLM. Data curation: JPC, JCM, RNR. Formal analysis: JPC, RNR, JMNA. Methodology: JPC, JCM, JMNA. Project administration: JPC, JRLM. Visualization: JPC, CAAL, JCM, RNR, JMNA, JRLM. Writing - original draft: JPC, JCM. Writing - review & editing: JPC, CAAL, RNR, JMNA, JRLM.
-
ACKNOWLEDGMENTS
None.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4266/acc.2023.01620.
Supplementary Figure 1.
Cardiogenic shock severity stages according to updated SCAI classification from Naidu et al. [7]. CS: cardiogenic shock; STEMI: ST-elevation myocardial infarction; LV: left ventricle; CKD: chronic kidney disease; SBP: systolic blood pressure; PAC: pulmonary artery catheter; CI: cardiac index; CVP: central venous pressure; PCWP: pulmonary capillary wedge pressure; SVO2: mixed venous oxygen saturation; MAP: mean arterial pressure; HR: heart rate; MCS: mechanical circulatory support; AKIN: Acute Kidney Injury Network NT-proBNP: N-terminal pro-brain natriuretic peptide.
acc-2023-01620-Supplementary-Figure-1.pdf
Figure 1.Patient inclusion flowchart. HF: heart failure; AMICS: acute myocardial infarction cardiogenic shock; SCAI: Society for Cardiovascular Angiography and Interventions.
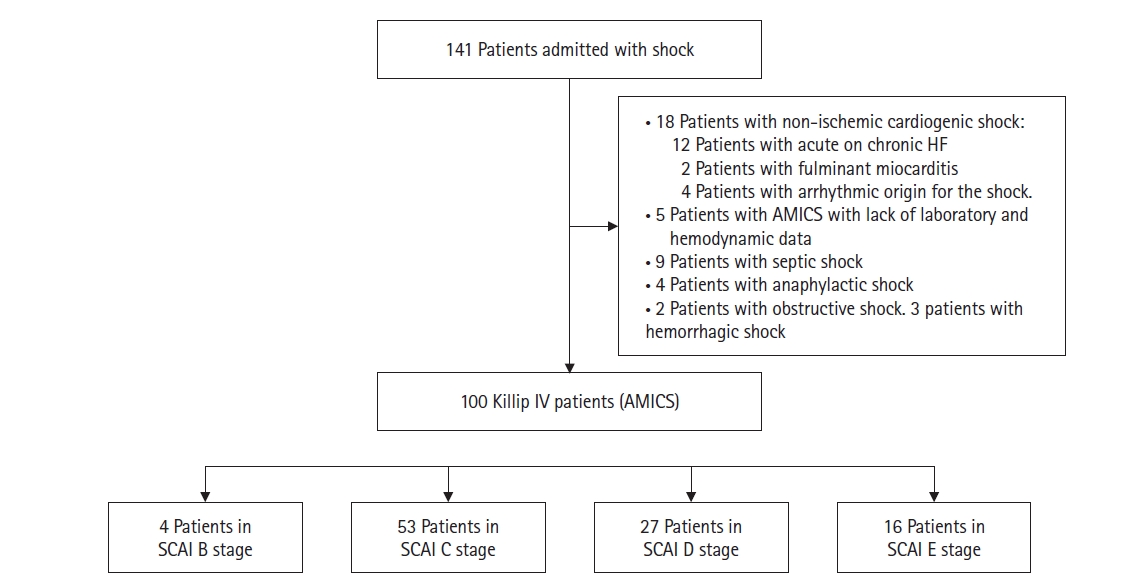
Figure 2.Kaplan-Meier plot showing progressive increase in 30-day mortality rate according to Society for Cardiovascular Angiography and Interventions (SCAI) stage and Killip IV stage.
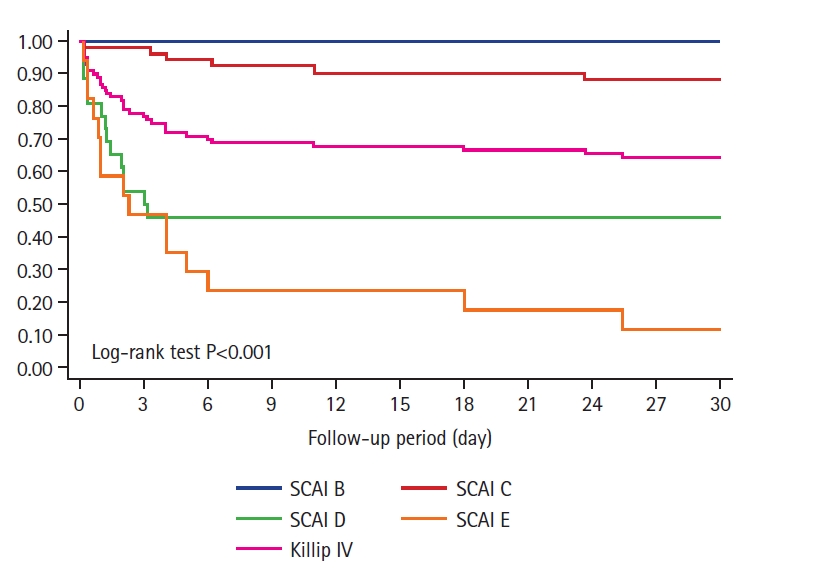
Figure 3.Comparison of 30-day mortality rate estimation between Killip IV stage and Society for Cardiovascular Angiography and Interventions (SCAI) C (A), D (B), and E (C) stages.
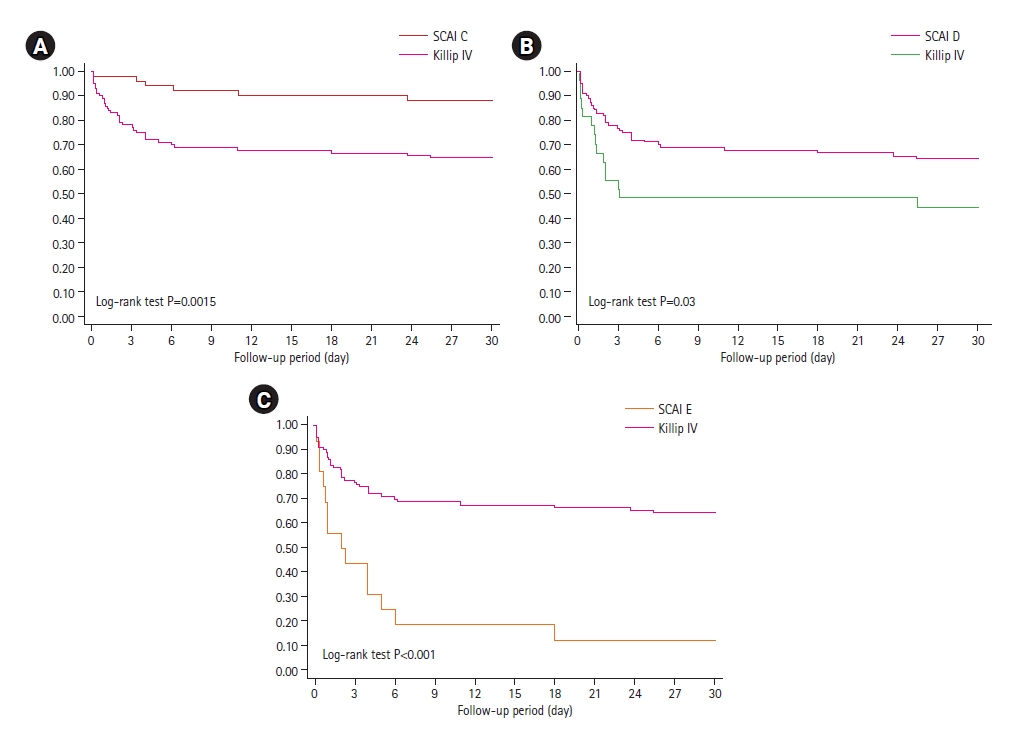
Figure 4.Kaplan-Meier curves showing impact of mechanical circulatory support (MCS) on survival in advanced Society for Cardiovascular Angiography and Interventions (SCAI) stages. HR: hazard ratio; CI: confidence interval.

Table 1.Demographic, clinical, analytical and echocardiographic features among different SCAI stages
|
Variable |
Killip IV (n=100) |
SCAI
|
P-value |
|
B (n=4) |
C (n=53) |
D (n=26) |
E (n=17) |
|
Demographic feature |
|
|
|
|
|
|
|
Male (%) |
68.0 |
50.0 |
71.7 |
61.5 |
70.6 |
0.67 |
|
Age (yr) |
66 (54–77) |
65 (60–68) |
63 (54–75) |
71 (50–80) |
67 (54–78) |
0.97 |
|
HTN (%) |
50.0 |
25.0 |
43.4 |
61.5 |
58.8 |
0.31 |
|
DLP (%) |
37.0 |
75.0 |
39.6 |
23.1 |
41.2 |
0.16 |
|
DM (%) |
28.0 |
25.0 |
20.8 |
30.8 |
47.1 |
0.19 |
|
Smoking habit (%) |
39.0 |
75.0 |
49.1 |
23.1 |
23.5 |
0.10 |
|
Clinical, analytical and echocardiographic features |
|
|
|
|
|
|
|
SBP (mm Hg) |
80.0 (70.0–90.0) |
72.5 (60.0–92.0) |
85.0 (80.0–95.0) |
74.5 (69.0–90.0) |
75.0 (70.0–80.0) |
0.03 |
|
Creatinine (mg/dl) |
1.3 (0.9–2.0) |
0.9 (0.8–1.0) |
1.1 (0.8–1.4) |
1.7 (1.3–2.6) |
3.1 (1.9–4.6) |
<0.001 |
|
AST (UI/L) |
331.5 (114.0–557.0) |
121.5 (91–211.0) |
183.0 (69.0–426.5) |
456.0 (111.0–724.0) |
460.0 (371.0–1,256.0) |
0.01 |
|
Lactate (mmol/L) |
3.5 (1.9–6.5) |
1.7 (1.7–1.7) |
2.4 (1.9–3.5) |
5.5 (3.8–8) |
7.0 (6.0–12.5) |
<0.001 |
|
LVEF (%) |
30.0 (20.0–41.0) |
50.0 (47.5–55.0) |
35.0 (25.0–40.0) |
30.0 (25.0–43.5) |
20.0 (15.0–22.5) |
<0.001 |
|
VIS |
20.0 (10.0–55.0) |
10.0 (10.0–10.0) |
12.5 (8.0–20.0) |
65.0 (22.0–98.5) |
79.5 (45.7–120.9) |
<0.001 |
|
OTI (%) |
60.0 |
25.0 |
52.8 |
61.5 |
88.2 |
0.02 |
|
OTI length (hr) |
48 (24–96) |
24 (24–24) |
48 (24–96) |
48 (24–96) |
48 (24–96) |
0.68 |
|
MCS (%) |
20.0 |
0 |
11.3 |
30.8 |
35.3 |
0.05 |
|
IABP (%) |
15.0 |
0 |
7.6 |
30.8 |
17.7 |
0.05 |
|
ECMO (%) |
4.0 |
0 |
0 |
11.5 |
5.9 |
0.07 |
|
Impella (%) |
5.0 |
0 |
2.2 |
0 |
17.7 |
0.10 |
|
LVEF at discharge (%) |
40 (32–50) |
58 (55–60) |
45 (35–50) |
35 (25–45) |
15 (10–30) |
<0.001 |
|
Length of stay (day) |
7.9 (2.3–14.4) |
5.3 (4.7–5.8) |
9.4 (6.2–13) |
3.1 (1.2–16.2) |
2.3 (0.8–6.0) |
0.03 |
Table 2.30-Day mortality predictors for patients in cardiogenic shock
|
Variable |
Univariate Cox regression
|
Multiple Cox regression
|
|
HR (95% CI) |
P-value |
HR (95% CI) |
P-value |
|
Age >69 yr |
2.95 (1.48–5.86) |
0.002 |
2.34 (1.15–4.76) |
0.019 |
|
Diabetes mellitus |
1.39 (0.99–1.95) |
0.056 |
– |
- |
|
AST >200 IU/L |
2.39 (1.08–5.27) |
0.031 |
- |
- |
|
VIS >20 |
4.31 (1.67–11.12) |
0.003 |
- |
- |
|
Lactate >3.5 mml/L |
10.16 (2.43–42.40) |
0.001 |
- |
- |
|
Creatinine >1.15 mg/dl |
30.43 (4.16–222.55) |
0.001 |
11.52 (1.43–92.77) |
0.022 |
|
LVEF <20% |
1.95 (0.96 –3.99) |
0.067 |
- |
- |
|
SCAI D stage |
2.56 (1.30–5.05) |
0.007 |
3.29 (1.20–9.01) |
0.020 |
|
SCAI E stage |
5.73 (2.90–11.32) |
<0.001 |
6.21 (2.28–16.88) |
<0.001 |
References
- 1. Kolte D, Khera S, Aronow WS, Mujib M, Palaniswamy C, Sule S, et al. Trends in incidence, management, and outcomes of cardiogenic shock complicating ST-elevation myocardial infarction in the United States. J Am Heart Assoc 2014;3:e000590.ArticlePubMedPMC
- 2. Berg DD, Bohula EA, van Diepen S, Katz JN, Alviar CL, Baird-Zars VM, et al. Epidemiology of shock in contemporary cardiac intensive care units. Circ Cardiovasc Qual Outcomes 2019;12:e005618.PubMedPMC
- 3. Thiele H, Akin I, Sandri M, Fuernau G, de Waha S, Meyer-Saraei R, et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med 2017;377:2419-32.ArticlePubMed
- 4. Hunziker L, Radovanovic D, Jeger R, Pedrazzini G, Cuculi F, Urban P, et al. Twenty-year trends in the incidence and outcome of cardiogenic shock in AMIS plus registry. Circ Cardiovasc Interv 2019;12:e007293.PubMed
- 5. Killip T 3rd, Kimball JT. Treatment of myocardial infarction in a coronary care unit: a two year experience with 250 patients. Am J Cardiol 1967;20:457-64.PubMed
- 6. Baran DA, Grines CL, Bailey S, Burkhoff D, Hall SA, Henry TD, et al. SCAI clinical expert consensus statement on the classification of cardiogenic shock: this document was endorsed by the American College of Cardiology (ACC), the American Heart Association (AHA), the Society of Critical Care Medicine (SCCM), and the Society of Thoracic Surgeons (STS) in April 2019. Catheter Cardiovasc Interv 2019;94:29-37.PubMed
- 7. Naidu SS, Baran DA, Jentzer JC, Hollenberg SM, van Diepen S, Basir MB, et al. SCAI SHOCK stage classification expert consensus update: a review and incorporation of validation studies. J Soc Cardiovasc Angiogr Interv 2022;1:100008. Article
- 8. Baran DA, Long A, Badiye AP, Stelling K. Prospective validation of the SCAI shock classification: single center analysis. Catheter Cardiovasc Interv 2020;96:1339-47.PubMedPMC
- 9. Schrage B, Dabboura S, Yan I, Hilal R, Neumann JT, Sörensen NA, et al. Application of the SCAI classification in a cohort of patients with cardiogenic shock. Catheter Cardiovasc Interv 2020;96:E213-9.ArticlePubMedPDF
- 10. Hanson ID, Tagami T, Mando R, Kara Balla A, Dixon SR, Timmis S, et al. SCAI shock classification in acute myocardial infarction: insights from the National Cardiogenic Shock Initiative. Catheter Cardiovasc Interv 2020;96:1137-42.PubMed
- 11. Wayangankar SA, Bangalore S, McCoy LA, Jneid H, Latif F, Karrowni W, et al. Temporal trends and outcomes of patients undergoing percutaneous coronary interventions for cardiogenic shock in the setting of acute myocardial infarction: a report from the CathPCI registry. JACC Cardiovasc Interv 2016;9:341-51.PubMed
- 12. Belletti A, Lerose CC, Zangrillo A, Landoni G. Vasoactive-inotropic score: evolution, clinical utility, and pitfalls. J Cardiothorac Vasc Anesth 2021;35:3067-77.ArticlePubMed
- 13. González-Pacheco H, Gopar-Nieto R, Araiza-Garaygordobil D, Briseño-Cruz JL, Eid-Lidt G, Ortega-Hernandez JA, et al. Application of the SCAI classification to admission of patients with cardiogenic shock: analysis of a tertiary care center in a middle-income country. PLoS One 2022;17:e0273086.ArticlePubMedPMC
- 14. Jentzer JC, van Diepen S, Barsness GW, Henry TD, Menon V, Rihal CS, et al. Cardiogenic shock classification to predict mortality in the cardiac intensive care unit. J Am Coll Cardiol 2019;74:2117-28.ArticlePubMed
- 15. Jentzer JC, Schrage B, Holmes DR, Dabboura S, Anavekar NS, Kirchhof P, et al. Influence of age and shock severity on short-term survival in patients with cardiogenic shock. Eur Heart J Acute Cardiovasc Care 2021;10:604-12.ArticlePubMedPDF
- 16. Schrage B, Becher PM, Goßling A, Savarese G, Dabboura S, Yan I, et al. Temporal trends in incidence, causes, use of mechanical circulatory support and mortality in cardiogenic shock. ESC Heart Fail 2021;8:1295-303.ArticlePubMedPMCPDF
- 17. Kim Y, Park J, Essa M, Lansky AJ, Sugeng L. Frequency of management of cardiogenic shock with mechanical circulatory support devices according to race. Am J Cardiol 2020;125:1782-7.ArticlePubMed
- 18. Berg DD, Kaur G, Bohula EA, Baird-Zars VM, Alviar CL, Barnett CF, et al. Prognostic significance of haemodynamic parameters in patients with cardiogenic shock. Eur Heart J Acute Cardiovasc Care 2023;12:651-60.ArticlePubMedPMCPDF
- 19. Harjola VP, Lassus J, Sionis A, Køber L, Tarvasmäki T, Spinar J, et al. Clinical picture and risk prediction of short-term mortality in cardiogenic shock. Eur J Heart Fail 2015;17:501-9.ArticlePubMed
- 20. Pöss J, Köster J, Fuernau G, Eitel I, de Waha S, Ouarrak T, et al. Risk stratification for patients in cardiogenic shock after acute myocardial infarction. J Am Coll Cardiol 2017;69:1913-20.ArticlePubMed
- 21. Damluji AA, Forman DE, van Diepen S, Alexander KP, Page RL 2nd, Hummel SL, et al. Older adults in the cardiac intensive care unit: factoring geriatric syndromes in the management, prognosis, and process of care: a scientific statement from the American Heart Association. Circulation 2020;141:e6-32.ArticlePubMed
- 22. Koreny M, Karth GD, Geppert A, Neunteufl T, Priglinger U, Heinz G, et al. Prognosis of patients who develop acute renal failure during the first 24 hours of cardiogenic shock after myocardial infarction. Am J Med 2002;112:115-9.ArticlePubMed
- 23. Ho HH, Ong HA, Arasaratnam P, Ooi YW, Tan J, Loh KK, et al. Predictors of in-hospital mortality in patients with acute myocardial infarction complicated by cardiogenic shock in the contemporary era of primary percutaneous coronary intervention. Int J Cardiol Heart Vessel 2014;3:88-9.ArticlePubMedPMC
- 24. Fuernau G, Poenisch C, Eitel I, Denks D, de Waha S, Pöss J, et al. Prognostic impact of established and novel renal function biomarkers in myocardial infarction with cardiogenic shock: a biomarker substudy of the IABP-SHOCK II-trial. Int J Cardiol 2015;191:159-66.ArticlePubMed
- 25. Zweck E, Kanwar M, Li S, Sinha SS, Garan AR, Hernandez-Montfort J, et al. Clinical course of patients in cardiogenic shock stratified by phenotype. JACC Heart Fail 2023;11:1304-15.ArticlePubMed
Citations
Citations to this article as recorded by

 , Carlos Antonio Aranda López1, Rosa Navarro Romero2, Javier Corral Macías2, Juan Manuel Nogales Asensio3
, Carlos Antonio Aranda López1, Rosa Navarro Romero2, Javier Corral Macías2, Juan Manuel Nogales Asensio3 , José Ramón López Mínguez3
, José Ramón López Mínguez3



 KSCCM
KSCCM
 PubReader
PubReader ePub Link
ePub Link Cite
Cite





