Articles
- Page Path
- HOME > Acute Crit Care > Volume 35(4); 2020 > Article
-
Original Article
Infection Risk factors for intensive care unit admission and mortality in hospitalized COVID-19 patients -
Ahmed Ayaz1
 , Ainan Arshad2
, Ainan Arshad2 , Hajra Malik1
, Hajra Malik1 , Haris Ali1
, Haris Ali1 , Erfan Hussain3
, Erfan Hussain3 , Bushra Jamil4
, Bushra Jamil4
-
Acute and Critical Care 2020;35(4):249-254.
DOI: https://doi.org/10.4266/acc.2020.00381
Published online: November 11, 2020
1Medical College, Aga Khan University, Karachi, Pakistan
2Department of Internal Medicine, Aga Khan University, Karachi, Pakistan
3Department of Pulmonary and Critical Care, Aga Khan University, Karachi, Pakistan
4Department of Infectious Diseases, Aga Khan University, Karachi, Pakistan
- Corresponding author Ainan Arshad Department of Internal Medicine, Aga Khan University, Faculty Office Building, Stadium Rd, Karachi 74800, Pakistan Tel: +92-21-33104123 Fax: +92-21-33104123 E-mail: ainan_arshad@hotmail.com
- *These authors contributed equally to this article.
Copyright © 2020 The Korean Society of Critical Care Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background
- This study investigated the clinical features and outcome of hospitalized coronavirus disease 2019 (COVID-19) patients admitted to our quaternary care hospital.
-
Methods
- In this retrospective cohort study, we included all adult patients with COVID-19 infection admitted to a quaternary care hospital in Pakistan from March 1 to April 15, 2020. The extracted variables included demographics, comorbidities, presenting symptoms, laboratory tests and radiological findings during admission. Outcome measures included in-hospital mortality and length of stay.
-
Results
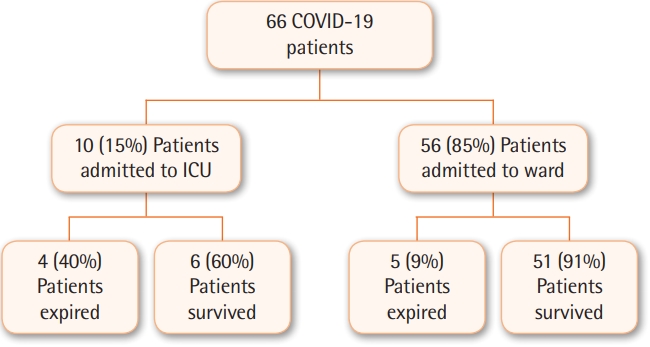
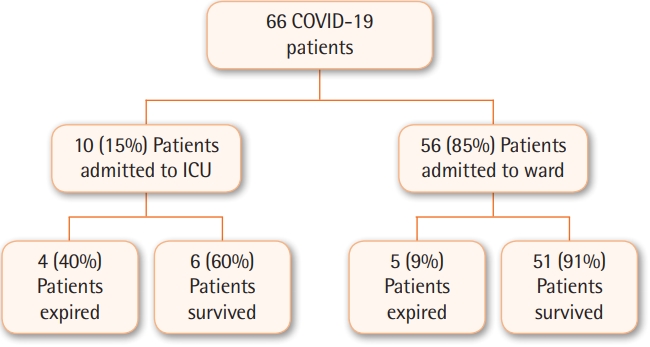
- Sixty-six COVID-19 patients were hospitalized during the study period. Sixty-one percent were male and 39% female; mean age was 50.6±19.1 years. Fever and cough were the most common presenting symptoms. Serial chest X-rays showed bilateral pulmonary opacities in 33 (50%) patients. The overall mortality was 14% and mean length of stay was 8.4±8.9 days. Ten patients (15%) required intensive care unit (ICU) care during admission, of which six (9%) were intubated. Age ≥60 years, diabetes, ischemic heart disease, ICU admission, neutrophil to lymphocyte ratio ≥3.3, and international normalized ratio ≥1.2 were associated with increased risk of mortality.
-
Conclusions
- We found a mortality rate of 14% in hospitalized COVID-19 patients. COVID-19 cases are still increasing exponentially around the world and may overwhelm healthcare systems in many countries soon. Our findings can be used for early identification of patients who may require intensive care and aggressive management in order to improve outcomes.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
DISCUSSION
KEY MESSAGES
-
CONFLICT OF INTEREST No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
Conceptualization: AA (Ahmed Ayaz), AA (Ainan Arshad), EH, BJ. Data curation: AA (Ainan Arshad), HM, HA. Formal analysis: AA (Ainan Arshad). Methodology: AA (Ahmed Ayaz), AA (Ainan Arshad). Project administration: AA (Ainan Arshad). Writing–original draft: AA (Ainan Arshad), HM, HA. Writing–review & editing: AA (Ainan Arshad), EH, BJ.
NOTES
Values are presented as number (%) or mean±standard deviation.
COVID-19: coronavirus disease 2019; Hb: hemoglobin; WBC: white blood cells; CRP: C-reactive protein; LDH: lactate dehydrogenase; AST: aspartate aminotransferase; ALT: alanine transaminase; PT: prothrombin time; PTT: partial thromboplastin time; INR: international normalized ratio.
- 1. Fauci AS, Lane HC, Redfield RR. Covid-19: navigating the uncharted. N Engl J Med 2020;382:1268-9.ArticlePubMedPMC
- 2. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020;382:1199-207.ArticlePubMedPMC
- 3. Open COVID-19 Data Curation Group. Novel corona virus (COVID-19)-healthMap [Internet]. Open COVID-19 Data Curation Group. 2020;[cited 2020 Nov 12]. Available from: https://www.healthmap.org/covid-19/.
- 4. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507-13.ArticlePubMedPMC
- 5. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020;395:1033-4.ArticlePubMedPMC
- 6. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708-20.ArticlePubMed
- 7. Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical characteristics of Covid-19 in New York City. N Engl J Med 2020;382:2372-4.ArticlePubMed
- 8. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020;323:1775-6.ArticlePubMed
- 9. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506.ArticlePubMedPMC
- 10. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061-9.ArticlePubMedPMC
- 11. Mao B, Liu Y, Chai YH, Jin XY, Lu HW, Yang JW, et al. Assessing risk factors for SARS-CoV-2 infection in patients presenting with symptoms in Shanghai, China: a multicentre, observational cohort study. Lancet Digit Health 2020;2:e323-30.ArticlePubMedPMC
- 12. Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology 2020;296:E32-40.ArticlePubMed
- 13. Huang P, Liu T, Huang L, Liu H, Lei M, Xu W, et al. Use of chest CT in combination with negative RT-PCR assay for the 2019 novel coronavirus but high clinical suspicion. Radiology 2020;295:22-3.ArticlePubMed
- 14. Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 2020;295:202-7.ArticlePubMed
- 15. Volpicelli G, Lamorte A, Villén T. What’s new in lung ultrasound during the COVID-19 pandemic. Intensive Care Med 2020;46:1445-8.ArticlePubMedPMC
- 16. Tang W, Cao Z, Han M, Wang Z, Chen J, Sun W, et al. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial. BMJ 2020;369:m1849. ArticlePubMedPMC
- 17. Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of Covid-19: final report. N Engl J Med 2020;383:1813-26.ArticlePubMed
- 18. Mahase E. Coronavirus covid-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ 2020;368:m641. ArticlePubMed
- 19. Gudbjartsson DF, Helgason A, Jonsson H, Magnusson OT, Melsted P, Norddahl GL, et al. Spread of SARS-CoV-2 in the Icelandic population. N Engl J Med 2020;382:2302-15.ArticlePubMed
- 20. Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA 2020;323:1612-4.ArticlePubMedPMC
- 21. Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, et al. Covid-19 in critically ill patients in the Seattle region: case series. N Engl J Med 2020;382:2012-22.ArticlePubMed
- 22. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis 2020;94:91-5.ArticlePubMedPMC
- 23. Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis 2020;34:101623. ArticlePubMedPMC
References
Figure & Data
References
Citations

- Healthcare-associated infection management in 62 ICUs for patients with congenital heart disease in China: a survey study
Xiaofeng Wang, Shuo Li, Da Huo, Shilin Wang, Wenlong Wang, Hongxia He, Qian Zhang, Jiantao Li, Xu Wang
International Journal of Surgery.2024; 110(4): 2025. CrossRef - Incidence and clinical outcomes of bacterial superinfections in critically ill patients with COVID-19
Si Mong Yoon, Jinwoo Lee, Sang-Min Lee, Hong Yeul Lee
Frontiers in Medicine.2023;[Epub] CrossRef - Difference in determinants of ICU admission and death among COVID-19 hospitalized patients in two epidemic waves in Portugal: possible impact of healthcare burden and hospital bed occupancy on clinical management and outcomes, March–December 2020
Vasco Ricoca Peixoto, André Vieira, Pedro Aguiar, Carlos Carvalho, Daniel Thomas, Paulo Sousa, Carla Nunes, Alexandre Abrantes
Frontiers in Public Health.2023;[Epub] CrossRef - Early Death Among COVID-19 Patients: A Cross-sectional Analysis of the First 10,000 COVID-19 Deaths from the Indian State of Tamil Nadu
Zarin Pilakkadavath, Janice M. Weinberg, Serin Kuriakose, Shahul H. Ebrahim, Lekha D. Bhat, Bindhya Vijayan, Salman Khan, Soji D. Jose, Premini Rajeev, Jinbert L. Azariah, Shaffi Fazaludeen Koya
Dr. Sulaiman Al Habib Medical Journal.2023; 5(4): 151. CrossRef - Global prevalence of COVID-19-induced acute respiratory distress syndrome: systematic review and meta-analysis
Abere Woretaw Azagew, Zerko Wako Beko, Yohannes Mulu Ferede, Habtamu Sewunet Mekonnen, Hailemichael Kindie Abate, Chilot Kassa Mekonnen
Systematic Reviews.2023;[Epub] CrossRef - Drinking patterns, alcoholic beverage types, and esophageal cancer risk in Africa: a comprehensive systematic review and meta-analysis
Eugene Jamot Ndebia, Gabriel Tchuente Kamsu
Frontiers in Oncology.2023;[Epub] CrossRef - The clinical association between Periodontitis and COVID-19
Shipra Gupta, Ritin Mohindra, Mohita Singla, Sagar Khera, Vaibhav Sahni, Poonam Kanta, Roop Kishor Soni, Amit Kumar, Krishan Gauba, Kapil Goyal, Mini P. Singh, Arnab Ghosh, Kamal Kajal, Varun Mahajan, Ashish Bhalla, Timo Sorsa, Ismo Räisänen
Clinical Oral Investigations.2022; 26(2): 1361. CrossRef - Prothrombin time, international normalized rate and in-hospital mortality in COVID-19
Panagiotis PALIOGIANNIS, Angelo ZINELLU, Arduino A. MANGONI, Antonio PAZZOLA, Francesco L. BANDIERA, Antonio SPANO, Chiara SANNA, Valentina SCANO, Sara S. FOIS, Verdiana MUSCAS, Elena MASOTTO, Stefano DORE, Vito FIORE, Pietro PIRINA, Ciriaco CARRU, Alessa
Minerva Respiratory Medicine.2022;[Epub] CrossRef - Patterns of presentation, prevalence and associated factors of mortality in ICU among adult patients during the pandemic of COVID 19: A retrospective cross-sectional study
Shimelis Seid, Habtu Adane, Getachew Mekete
Annals of Medicine and Surgery.2022; 77: 103618. CrossRef - Hospital length of stay for COVID-19 patients: A systematic review and meta-analysis
Yousef Alimohamadi, Elahe Mansouri Yekta, Mojtaba Sepandi, Maedeh Sharafoddin, Maedeh Arshadi, Elahe Hesari
Multidisciplinary Respiratory Medicine.2022;[Epub] CrossRef - Evaluation of the models generated from clinical features and deep learning-based segmentations: Can thoracic CT on admission help us to predict hospitalized COVID-19 patients who will require intensive care?
Mutlu Gülbay, Aliye Baştuğ, Erdem Özkan, Büşra Yüce Öztürk, Bökebatur Ahmet Raşit Mendi, Hürrem Bodur
BMC Medical Imaging.2022;[Epub] CrossRef - Characterization and determinant factors of critical illness and in-hospital mortality of COVID-19 patients: A retrospective cohort of 1,792 patients in Kenya
Isinta M Elijah, Endawoke Amsalu, Xuening Jian, Mingyang Cao, Eric K Mibei, Danvas O Kerosi, Francis G Mwatsahu, Wei Wang, Faith Onyangore, Youxin Wang
Biosafety and Health.2022; 4(5): 330. CrossRef - SARS-CoV-2-Infection (COVID-19): Clinical Course, Viral Acute Respiratory Distress Syndrome (ARDS) and Cause(s) of Death
Giuliano Pasquale Ramadori
Medical Sciences.2022; 10(4): 58. CrossRef - Risk factors for SARS-CoV-2 related mortality and hospitalization before vaccination: A meta-analysis
Hannah N. Marmor, Mindy Pike, Zhiguo (Alex) Zhao, Fei Ye, Stephen A. Deppen, Julio Croda
PLOS Global Public Health.2022; 2(11): e0001187. CrossRef - Risk factors of early mortality among COVID-19 deceased patients in Addis Ababa COVID-19 care centers, Ethiopia
Taye Ashine Mezgebu, Migbar Mekonnen Sibhat, Melsew Tsegaw Getnet, Kassie Tiruneh Gebeyehu, Wuletaw Zewde Chane, Edmialem Mesfin Getahun, Asaminew Sane Habtamu, Hailu Beyene Asmare, Melke Mengistie Ambaw, Zivanai Cuthbert Chapanduka
PLOS ONE.2022; 17(9): e0275131. CrossRef - Comorbid Asthma Increased the Risk for COVID-19 Mortality in Asia: A Meta-Analysis
Liqin Shi, Jiahao Ren, Yujia Wang, Huifen Feng, Fang Liu, Haiyan Yang
Vaccines.2022; 11(1): 89. CrossRef - Outcomes of nutritionally at-risk Coronavirus Disease 2019 (COVID 19) patients admitted in a tertiary government hospital: A follow-up study of the MalnutriCoV study
Ramon B. Larrazabal, Harold Henrison C. Chiu, Lia Aileen M. Palileo-Villanueva
Clinical Nutrition ESPEN.2021; 43: 239. CrossRef - Prognostic value of neutrophil‐to‐lymphocyte ratio in COVID‐19 patients: A systematic review and meta‐analysis
Juan R. Ulloque‐Badaracco, W. Ivan Salas‐Tello, Ali Al‐kassab‐Córdova, Esteban A. Alarcón‐Braga, Vicente A. Benites‐Zapata, Jorge L. Maguiña, Adrian V. Hernandez
International Journal of Clinical Practice.2021;[Epub] CrossRef - A meta-analysis on the risk factors adjusted association between cardiovascular disease and COVID-19 severity
Jie Xu, Wenwei Xiao, Xuan Liang, Li Shi, Peihua Zhang, Ying Wang, Yadong Wang, Haiyan Yang
BMC Public Health.2021;[Epub] CrossRef - Comparison of characteristics and ventilatory course between coronavirus disease 2019 and Middle East respiratory syndrome patients with acute respiratory distress syndrome
Imran Khalid, Romaysaa M Yamani, Maryam Imran, Muhammad Ali Akhtar, Manahil Imran, Rumaan Gul, Tabindeh Jabeen Khalid, Ghassan Y Wali
Acute and Critical Care.2021; 36(3): 223. CrossRef
- Figure
- Related articles
-
- Factors related to lung function outcomes in critically ill COVID-19 patients in South Korea
- Prolonged intensive care: muscular functional, and nutritional insights from the COVID-19 pandemic
- Predicting factors associated with prolonged intensive care unit stay of patients with COVID-19
- Comment on “Risk factors for intensive care unit readmission after lung transplantation: a retrospective cohort study”
- An algorithm to predict the need for invasive mechanical ventilation in hospitalized COVID-19 patients: the experience in Sao Paulo

 KSCCM
KSCCM
 PubReader
PubReader ePub Link
ePub Link Cite
Cite