Abstract
-
Background
- Korea is rapidly becoming a super aging society and is facing the increased burden of critical care for the elderly people. Traditionally, far-advanced age has been regarded as a triage criterion for intensive care unit (ICU) admission. We evaluated how the characteristics and prognostic factors of very elderly patients (≥85 years) admitted to the ICU changed over the last decade.
-
Methods
- We retrospectively evaluated the data of patients admitted to the ICU over 11 years (2007–2017). The clinical characteristics and outcomes of the very elderly-patients group were evaluated. Factors associated with mortality were assessed by a cox regression analysis.
-
Results
- Comparing the first half (2007–2012) and the second half (2013–2017) of the study period, the proportion of very elderly group increased from 603/47,657 (1.3%), to 697/37,756 (1.8%) (P<0.001). Among 1,294 very elderly patients, 1,274 patients were analyzed excluding hopeless discharge (n=20). The non-surgical reasons for ICU admission (67.0% vs. 76.1%, P<0.001) and the percentage of patients with co-morbidities (78.3% vs. 82.7%, P=0.048) were increased. Nevertheless, the hospital mortality decreased (21.3% vs. 14.9%, P=0.001). High creatinine levels, use of vasopressors and ventilator weaning failure were associated with in-hospital mortality.
-
Conclusions
- The proportion of very elderly people in the ICU increased over the last decade. The non-surgical causes of ICU admission increased compared with the surgical causes. Despite an increasement in ICU admissions of very elderly patients, in-hospital mortality of very elderly ICU patients decreased.
-
Keywords: aging society; critical care; mortality; very elderly
INTRODUCTION
The Republic of Korea is growing into an aging society. In Korea, the proportion of the elderly population (65 and older) increased from 11.5% in 2012 to 16.5% in 2021. Additionally, the aging index (the number of elderly people [≥65 years] per 100 individuals younger than 14 years in a specific population) also rapid increased from 76.1% in 2012 to 138.8% in 2021 [1]. Considering the current trend of population change, it is high probable that Korea becomes a super aging society by 2029 [2]. Older age is associated with a higher prevalence of chronic diseases and a higher incidence of hospital admission and intensive care unit (ICU) treatment [3].
ICU and in-hospital mortalities in elderly patients are higher than those in non-elderly patients [4-7]. In a study of very elderly (≥80 years) patients admitted to the medical ICU in Korea, weaning failure and the withdrawal, or withholding of intensive care in the ICU were significantly related to death in patients ≥ 80 years old [8]. In addition, male sex and moderate malnutrition were factors associated with mortality in a study involving patients aged ≥65 years admitted to the ICU without limitations on other therapeutic efforts [9]. However, the clinical characteristics and prognostic factors of very elderly patients admitted to the ICU and changes in the characteristics of the patient population over time in the aging society are not well known.
In this study, we investigated the clinical characteristics of very elderly patients (over 85 years of age) in our ICU over the last decade and compared the first half (2007–2012) and the second half (2013–2017) of the study period. We aimed to determine if age ≥85 years should be regarded as an exclusion criterion in the ICU triage.
MATERIALS AND METHODS
Study Population and Study Design
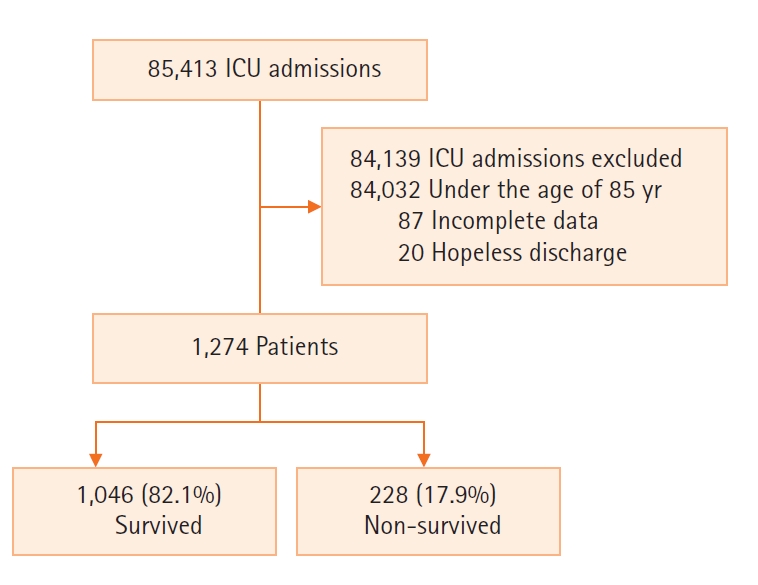
Between January 1, 2007, and December 31, 2017, 85,413 patients aged ≥18 years were enrolled. Patients under the age of 85 (n=84,032), patients with missing data (n=87), hopeless discharge (n=20) were excluded (Figure 1). This retrospective single-center cohort study was conducted in an ICU with 28 medical beds, 26 general surgical beds, 13 neurological beds, 14 neurosurgical beds, 16 cardiovascular beds, 15 cardiac surgical beds, and 10 emergent beds at a tertiary care hospital in Seoul, Korea. Each ICU had a dedicated intensivist and/or a fellow 24 hours a day to attend to the patients.
All the study data were retrieved from electronic medical records (Medical Information System 2.0, Seoul, Korea). Basic demographic characteristics including sex, age, type of admission (medical, surgical), length of hospital stay, length of ICU stay, ICU admission diagnosis, need for invasive support (mechanical ventilation and renal replacement therapy [RRT]) and vasopressors on ICU admission and during ICU stay, Sequential Organ Failure Assessment (SOFA) scores, in-hospital mortality, and mortality at ICU discharge were analyzed. Patients over 85 years of age were defined as very elderly. The first half of the study period was defined as 2007 to 2012, and the second half was defined as 2013 to 2017. SOFA scores during the first 24 hours of ICU admission were also assessed for mortality prediction. SOFA scores were based on a study by Vincent et al. [10]. The worst value for each organ system in every 24 hours was chosen to calculate the score.
This study was approved by the Institutional Review Board of Asan Medical Center (No. 2018-0431), and the requirement to obtain informed consent was waived due to the retrospective nature of the study.
Statistical Analysis
All values are expressed as means±standard deviations for continuous variables and as percentages for categorical variables. Student t-test or Mann-Whitney U-test was performed for continuous data, and Pearson’s chi-square test or Fisher’s exact test was performed for categorical data. The trend according to year was analyzed through linear-by-linear association. A univariate cox regression analysis and multivariate cox regression analysis were performed to identify the predictors of in-hospital mortality. All P-values were two-tailed, with statistical significance set at a P-value of <0.05. All statistical analyses were performed using IBM SPSS version 22.0 (IBM Corp., Armonk, NY, USA).
RESULTS
Patients’ Baseline Characteristics
During the study period, there were 85,413 ICU admissions (Figure 1). Of 1,274 patients included in this study, 1,046 (82.1%) patients survived, and 228 (17.9%) patients died upon discharge from hospital. The mean age of the patients was 87.8±2.9 years, and 47.3% of them were male. Of the ICU admissions, 71.9% were for medical reasons, and the most common reason for admission was cardiovascular disease. Furthermore, 28.1% of the ICU admissions were for surgical reasons, and the most common reason for admission was gastrointestinal & hepatobiliary disease. The ICU mortality was 12.8%, length of stay (LOS) in the ICU was 3.0 days (interquartile range, 1.0–6.0 days), and in-hospital mortality was 17.9%.
Differences between the First Half (2007–2012) and the Second Half (2013–2017) of the Study Period
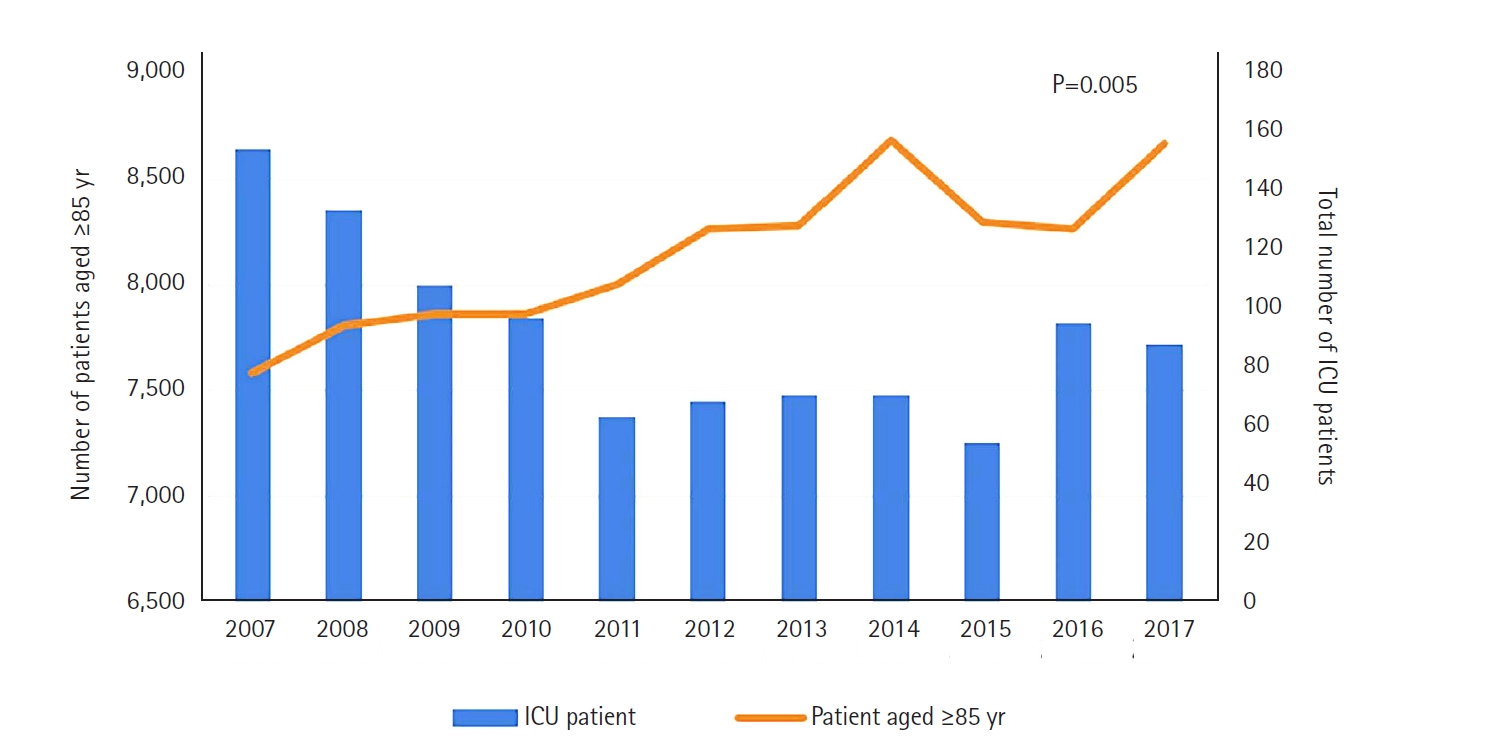
Among the patients admitted to the ICU, the proportion of those aged ≥85 years increased from 0.9% in 2007 to 2.0% in 2017 ((including do-not-resuscitate [DNR] and hopeless discharge) (Figure 2). The proportion of the very elderly group increased from 603/47,657 (1.3%) in the first half (2007–2012) to 697/37,756 (1.8%) (P<0.001) in the second half (2013–2017) of the study period. The patients' baseline characteristics are shown in Table 1. Compared with the first half period, the mean SOFA score in the second half period was lower (second half vs. first half: 13.9±4.4 vs. 14.5±4.5, P=0.033), the percentage of medical reasons for admission to the ICU increased (76.1% vs. 67.0%, P<0.001), and the percentage of surgical reasons decreased (23.9% vs. 33.0%, P<0.001). The number of admissions from the ward to the ICU increased, and those to the emergency room decreased (P=0.041). Compared with the first half period, the number of co-morbidities in the second half period are as follows (second half vs. first half: 82.7% vs. 78.3%, P=0.048). Hypertension: 467 (68.4%) vs. 373 (63.1%), P=0.048; chronic heart disease: 179 (26.2%) vs. 102 (17.3%), P<0.001; solid tumor: 45 (6.6%) vs. 18 (3.0%), P=0.004; and, cerebrovascular accident: 92 (13.5%) vs. 55 (9.3%), P=0.020. Regarding nonoperative admission diagnoses, infection (4 [0.8%] vs. 9 [2.3%], P=0.057) decreased and other reasons (like rehabilitation, psychiatry, endocrinology, and emergency medicine) (106 [20.4%] vs. 56 [14.1%], P=0.014) increased. Operative admission diagnoses showed an increase in gastrointestinal and hepatobiliary diagnoses (59 [36.2%] vs. 50 [25.6%], P=0.031) and a decrease in orthopedic diagnoses (15 [9.2%] vs. 50 [25.6%], P<0.001).
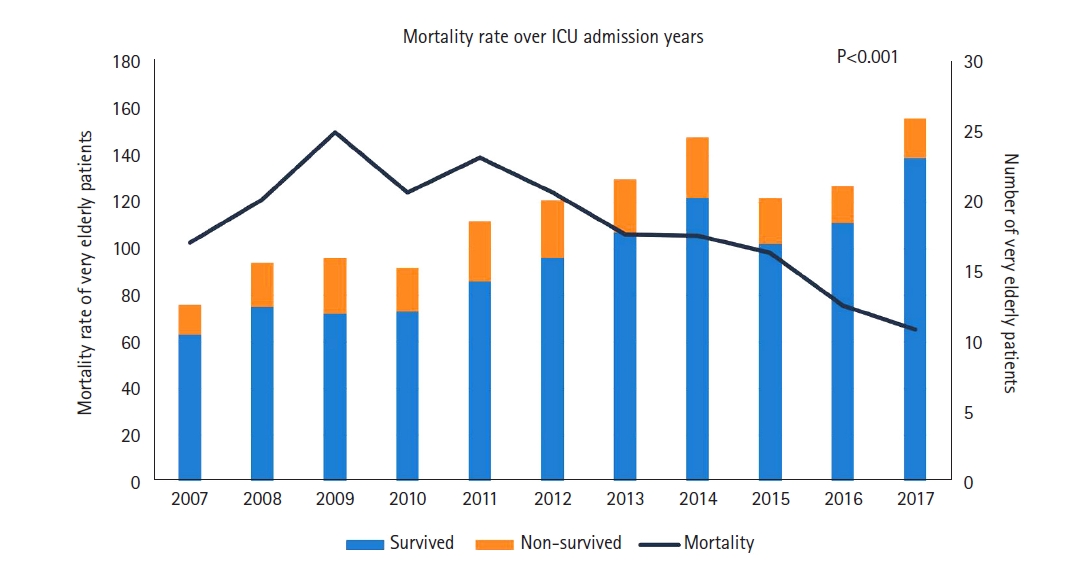
The resource use and outcomes in the first and the second halves of the study period have been described (Table 2). The use of vasopressors (35.1% vs. 29.4%, P=0.030) increased in the second half. After adjusting for the SOFA score, reason for admission to ICU, hypertension, chronic heart disease, solid tumor, and cerebrovascular accident among the underlying diseases, in-hospital mortality (14.9% vs. 21.3%, P=0.001) decreased. And hospital LOS decreased. There were reductions in the number of patients who did not survive and in the in-hospital mortality during the study period (P<0.001) (Figure 3).
Comparison between Survived and Non-survived Groups
The characteristics of the studied patients are provided (Supplementary Table 1). In the non-survived group, there were more male (54.4% vs. 45.8%, P=0.019) and more patients admitted to the ICU for medical reasons (81.6% vs. 69.8%, P<0.001) than the survived group. Compared with the survived group, non-survived group showed high white blood cell (white blood cell: 11.6 ×103/µl [7.8–17.0] vs. 9.5 ×103/µl [7.0–12.5], P<0.001), total bilirubin (0.8 mg/dl [0.6–1.3] vs. 0.8 mg/dl [0.5–1.1], P=0.002), creatinine (1.50 mg/dl [0.90–2.30] vs. 0.99 mg/dl [0.76–1.38], P<0.001), and C-reactive protein (5.33 ng/ml [1.32–14.34] vs. 1.87 ng/ml [0.31–7.23], P<0.001) levels, and low platelet (169 ×103/ul [106–229] vs. 186 ×103/ul [139–241], P=0.040), albumin (2.6 g/dl [2.0–3.2] vs. 2.9 g/dl [2.5–3.4], P<0.001) levels. Regarding underlying diseases, hematologic malignancies (1.3% vs. 0%, P<0.001) and diabetes mellitus (31.6% vs. 25.2%, P=0.049) were more common in the non-survived group.
Regarding the nonoperative admission diagnoses, the frequencies of cardiovascular (26.9% vs. 42.1%, P<0.001), neurologic (8.1% vs. 13.8%, P=0.035) were less and those of respiratory disease (39.2% vs. 12.6%, P<0.001), infection (3.8% vs 0.8%, P=0.002), and hematologic disease (1.1% vs. 0%, P=0.005) were more common in the non-survived group. In the operative diagnoses, gastrointestinal & hepatobiliary was more common in the non-survived group (45.2% vs. 28.5%, P=0.027) (Supplementary Table 2). The use of resources, expressed as the need for invasive mechanical ventilation, vasopressors, and RRT were higher in the non-survived group than that in the survived group (Supplementary Table 3). Compared with the survived group, the ICU LOS was longer in the non-survived group (Supplementary Table 3).
Predictors of Patients’ In-hospital Mortality
A cox regression analysis of the factors associated with in-hospital mortality was conducted (Table 3). After adjusting for confounders, the independent predictors of in-hospital mortality included admission source (compared with ward), emergency room (odds ratio [OR], 1.970; 95% confidence interval [CI], 1.247–3.112; P=0.004), others (OR, 2.220; 95% CI, 0.837–5.883; P=0.109); high creatinine level (OR, 1.234; 95% CI, 1.085–1.402; P=0.001); ventilator weaning (OR, 0.064; 95% CI, 0.036–0.115; P<0.001) and use of vasopressors (OR, 1.550; 95% CI, 1.004–2.394; P=0.048) (Table 3).
DISCUSSION
On comparing the first half (2007–2012) and the second half (2013–2017) of the study period, the proportion of the very elderly group increased, and the number of patients with underlying disease are increased, but the in-hospital mortality decreased. There were more males in the non-survived group, and there were more medical reasons for admission to the ICU. In addition, mechanical ventilation, vasopressors, and RRT were more required in the non-survived group than in the survived group. High creatinine level, ventilator weaning failure and use of vasopressors were associated with in-hospital mortality.
In Korea and other countries around the world, the proportion of the elderly population is increasing rapidly, and the number of elderly people in need of intensive care is also increasing [1,11-14]. In Korea, a rapidly aging society, there are few studies conducted in very elderly patients admitted to the ICU [14-16]. According to data from 38 ICU training hospitals, 3.7% of patients admitted to the ICU are aged ≥85 years [15]. Additionally, Lee et. al. [8] reported that 21.7% of patients admitted to the ICU were aged ≥80 years. Furthermore, Kim et al. [16] showed that 0.5%–1.9% of patients admitted to the ICU were over 90 years old. In our study, 0.9%–2.0% of the patients admitted to the ICU were ≥85 years old from 2007 to 2017. It is predicted that the number of very elderly patients in the ICU will increase, which is related to the increase in life expectancy in each country [11]. Each study showed various percentages of very elderly patients admitted to the ICU. This may have been influenced by the fact that the age of the study subjects, defined as very elderly patients, varied as 80, 85, and 90 years old, and the ratio of very elderly patients according to the life expectancy of each country varied by period.
The number of very elderly people admitted to the ICU is steadily increasing. As the number of very elderly patients admitted to the ICU increases, there is a change in the patients’ underlying disease and prognosis. On comparing the first half (2007–2012) and the second half (2013–2017) of the study period, the number of ICU admissions for medical reasons increased. During the second half of the study period, the number of underlying diseases such as hypertension, chronic heart disease, solid tumor, and cerebrovascular accident increased. However, in-hospital mortality and hospital LOS decreased in the second half of the study period. Kim et al. [16] reported slight increases in hypertension and cardiogenic shock, among the underlying diseases, as reasons for ICU admission in 2010–2014 compared with that in 2005–2009. Additionally, the mortality rate decreased from 2005 to 2014. In Kim et al.'s study [16] of patients admitted to the medical ICU from 2003 to 2013, the number of patients over 80 years of age increased from 7.3% in 2002 to 23.1% in 2013. However, there was no difference in the annual survival probability according to year (P=0.895) [17]. In Korea, there is a greater interest in intensivists and nursing staff working in the ICU than before, and the presence of intensivists [18] and the number of nursing staff [19] are known to be associated with lower mortality. In addition, there is a tendency for mortality to decrease in acute respiratory distress syndrome [20] and sepsis [21], which are related to mortality in the elderly. These points may have influenced the pattern of decreasing mortality in this study.
In this study, in the very elderly patients admitted to the ICU, hematologic malignancy, diabetes mellitus (DM) were more common in the non-survived group. In addition, in the non-survived group, white blood cell, total bilirubin, creatinine, and C-reactive protein levels were higher, and albumin level was lower than those in the survived group. Additionally, invasive mechanical ventilation and RRT were performed more often in the non-survived group. Roch et al. [22] showed that in-hospital non-survivors, the Simplified Acute Physiology Score (SAPS) II and the SOFA score were higher, and mechanically ventilation and RRT were often performed. Lee et al. [8] showed that the SOFA and Acute Physiology And Chronic Health Evaluation (APACHE) II scores were higher, and renal disease and rates of severe sepsis and septic shock were more common in the non-survivor group. Higher SAPS II [7], SOFA scores [23], and APACHE scores [24] mean that the non-survivor patients were severely ill; thus, treatments such as invasive mechanical ventilation and RRT are more likely to be required.
In the non-survived group, there were more respiratory, infection-related, and hematologic reasons for medical ICU admission. Kim et al. [16] reported that the most common reason for ICU care was acute respiratory failure. Many functional, demographic, and immunologic changes associated with aging are responsible for the increasing incidence and severity of infectious diseases in the elderly [25]. Martin-Loeches et al. [26] showed very elderly patients with sepsis had more pneumonia than elderly patients.
Older age is well-known factor associated with in-hospital mortality in patients admitted to the ICU. However, there are few studies on the characteristics of very elderly patients in the ICU (≥85 years). Lee et al. [8] showed that weaning failure and the withdrawal or withholding of intensive care in the ICU were significantly related to mortality in patients age ≥80 years. Martin-Loeches et al. [26] showed that patients aged ≥80 with sepsis had higher hospital mortality compared with patients aged between 65 and 79 years. In the group of very elderly patients, the predictors of hospital mortality were age, APACHE II score, and prompt adherence to the resuscitation bundle. Giannasi et al. [9] showed that after adjusting for APACHE II score and age, the following independent variables were associated with mortality: male sex, moderate malnutrition, severe malnutrition, and activities of daily living scores <6. Mukhopadhyay et al. [27] showed that in the elderly group, neurological disease, malignancy, mortality prediction model II score, mechanical ventilation, non-invasive ventilation, vasopressor use, and prior RRT were associated with in-hospital mortality. Considering long-term mortality as a prognosis, Atramont et al. [28] showed that age and reason for hospitalization were strongly associated with long-term mortality (9-, 13-, and 20-fold increases in the risk of death 3 years after ICU discharge in patients aged 80–84, 85–89, and ≥90 years, respectively). In this study, like other studies, high creatinine level, ventilator weaning failure and use of vasopressors were associated with in-hospital mortality. The patient's underlying disease was not associated with in-hospital mortality in this study. There was no significant difference in comorbidities except for hematologic malignancy, DM between the survived group and the non-survived group, so it seems to have a influenced the absence of statistically significant risk factor. In some studies, comorbidities did not show as a significant factor even in the elderly. In a systematic review of older patients (≥75 years) by Vallet et al. [29], ICU mortality and comorbidities were associated with one out of six studies, and in-hospital mortality and comorbidities were associated with 10 out of 12 studies. In a review by de Rooij et al. [30], comorbidities are common in very elderly patients, but the effect on outcome is not clearly shown. Therefore, in very elderly patients, ICU management is recommended considering the severity of the patient, the reason for ICU admission, and the functional status in addition to the comorbidities. Therefore, in very elderly patients, it is necessary to help in making a treatment decision considering various factors such as frailty, severity, and laboratory data in addition to comorbidities.
There are some limitations to our study. First, it was a single-center retrospective study and does not represent the entire Korean ICU population. Second, there is a possibility of selection bias as we did not collect data on the ICU’s denial of admission and/or patient/doctor preferences. Therefore, we were unable to estimate the gradual benefits of ICU support for those very old patients rejected admission to the ICU. Third, there is no information about the patients’ functional statuses prior to hospitalization. For elderly patients, the evaluation of the pre-hospital functional status is important, but data could not be collected because the patients’ previous functional evaluations were not clear in the electronic medical records. Fourth, we did an analysis that included patients with documented DNR. In actual situations, there are cases where DNR was received in verbal form or in patients with imminent death who received DNR to avoid cardiopulmonary compression. We were not able to collect additional data of DNR. Therefore, we were unable to conduct a separate analysis on the effect of DNR on patients.
In conclusion, the proportion of very elderly people (≥85 years) in the ICU has increased over the last decade (from 2007 to 2017). In the very elderly admitted in the ICU, the number of patients with underlying diseases slightly increased, but the prognosis was improved. In addition to age, laboratory data and disease severity contribute to patient outcomes. Therefore, we need to consider various factors in addition to age to determine ICU management for very elderly patients.
KEY MESSAGES
▪ The proportion of very elderly patients in the intensive care unit (ICU) increased from 1.3% to 1.8%.
▪ Non-surgical causes of ICU admission and the number of patients with underlying diseases were increased, and in-hospital mortality decreased from 2007 through 2017.
▪ High creatinine levels, use of vasopressors and ventilator weaning failure in the ICU were significantly associated with death in patients aged ≥85 years.
NOTES
-
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
Conceptualization: all authors. Data curation: SIL, CML. Validation: SIL, CML. Verification: SIL, CML. Visualization: SIL. Formal analysis: SIL, CML. Methodology: SIL, CML. Writing–original draft: SIL. Writing–review & editing: CML, YSK, JWH, SBH.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.4266/acc.2022.00066.
Figure 1.Flowcharts of patients. ICU: intensive care unit.
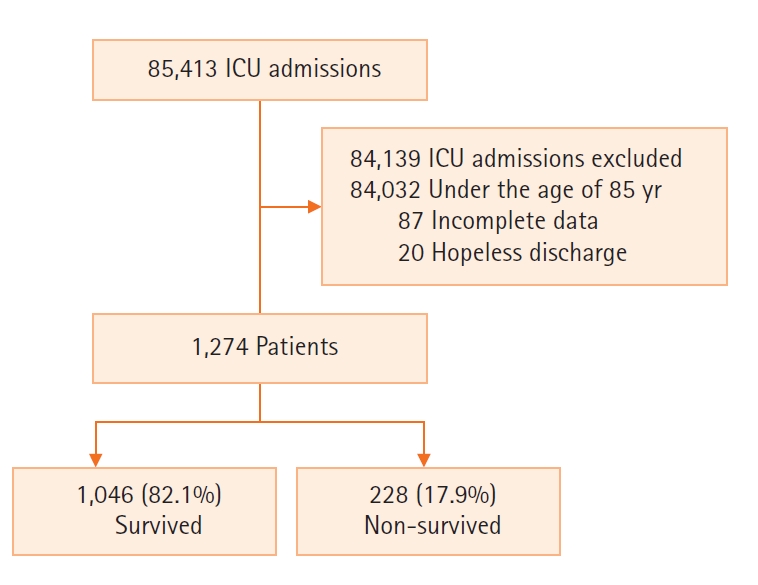
Figure 2.Number of all patients in the intensive care unit (ICU) and very elderly (aged ≥85 years) patients by year including do-not-resuscitate (DNR) and hopeless discharge.
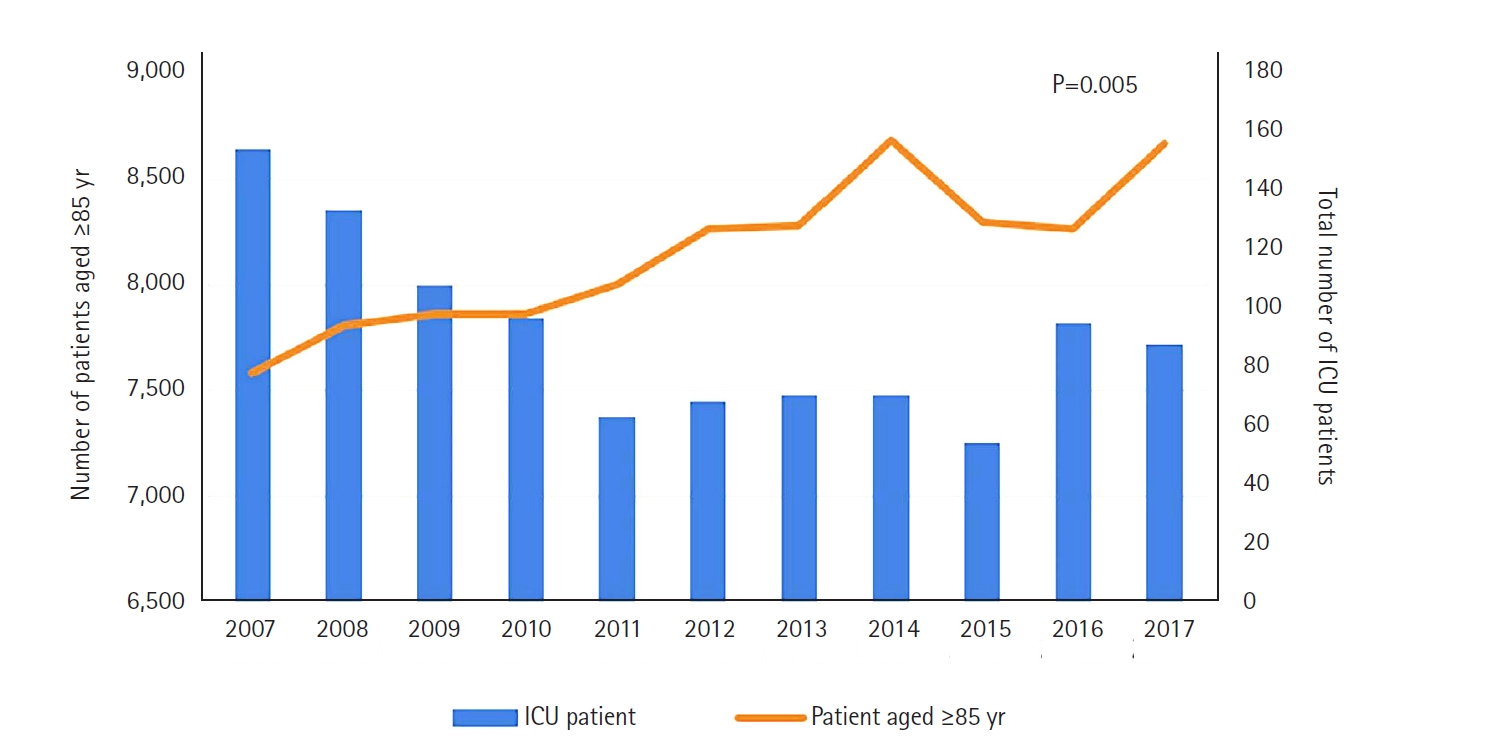
Figure 3.Number of survived and non-survived very elderly patients in the intensive care unit (ICU) and mortality by year.

Table 1.Characteristics of study participants according to period
|
Characteristics |
All patients |
2007–2012 |
2013–2017 |
P-value |
|
No. of patients |
1,274 |
591 |
683 |
|
|
Age (yr) |
87.8±2.9 |
87.7±2.8 |
87.9±3.0 |
0.243 |
|
Men |
603 (47.3) |
292 (49.4) |
311 (45.5) |
0.167 |
|
SOFA score |
14.2±4.4 |
14.5±4.5 |
13.9±4.4 |
0.033 |
|
Reason for index ICU admission |
|
|
|
|
|
Medical |
916 (71.9) |
396 (67.0) |
520 (76.1) |
<0.001 |
|
Surgical |
358 (28.1) |
195 (33.0) |
163 (23.9) |
<0.001 |
|
Admission source |
|
|
|
0.041 |
|
Ward |
298 (23.4) |
121 (20.5) |
177 (25.9) |
|
|
Emergency room |
945 (74.2) |
458 (77.5) |
487 (71.3) |
|
|
Others |
31 (2.4) |
12 (2.0) |
19 (2.8) |
|
|
Underlying disease |
1,028 (80.7) |
463 (78.3) |
565 (82.7) |
0.048 |
|
Hypertension |
840 (65.9) |
373 (63.1) |
467 (68.4) |
0.048 |
|
Chronic heart disease |
281 (22.1) |
102 (17.3) |
179 (26.2) |
<0.001 |
|
Hematologic malignancy |
3 (0.2) |
2 (0.3) |
1 (0.1) |
0.481 |
|
Solid tumor |
63 (4.9) |
18 (3.0) |
45 (6.6) |
0.004 |
|
Chronic liver disease |
10 (0.8) |
6 (1.0) |
4 (0.6) |
0.386 |
|
Chronic lung disease |
81 (6.4) |
36 (6.1) |
45 (6.6) |
0.717 |
|
DM |
336 (26.4) |
159 (26.9) |
177 (25.9) |
0.690 |
|
CKD |
46 (3.6) |
17 (2.9) |
29 (4.2) |
0.191 |
|
CVA |
147 (11.5) |
55 (9.3) |
92 (13.5) |
0.020 |
|
Nonoperative admission diagnoses |
|
|
|
|
|
Cardiovascular |
357 (39.0) |
152 (38.4) |
205 (39.4) |
0.749 |
|
Respiratory |
165 (18.0) |
82 (20.7) |
83 (16.0) |
0.064 |
|
Gastrointestinal & hepatobiliary |
81 (8.8) |
39 (9.8) |
42 (8.1) |
0.350 |
|
Nephrological |
16 (1.7) |
8 (2.0) |
8 (1.5) |
0.581 |
|
Oncologic |
4 (0.4) |
3 (0.8) |
1 (0.2) |
0.199 |
|
Infection |
13 (1.4) |
9 (2.3) |
4 (0.8) |
0.057 |
|
Hematologic |
2 (0.2) |
2 (0.5) |
0 |
0.105 |
|
Neurologic |
116 (12.7) |
45 (11.4) |
71 (13.7) |
0.302 |
|
Othersa
|
162 (17.7) |
56 (14.1) |
106 (20.4) |
0.014 |
|
Operative admission diagnoses |
|
|
|
|
|
Cardiovascular |
89 (24.9) |
45 (23.1) |
44 (27.0) |
0.393 |
|
Gastrointestinal & hepatobiliary |
109 (30.4) |
50 (25.6) |
59 (36.2) |
0.031 |
|
Orthopedic |
65 (18.2) |
50 (25.6) |
15 (9.2) |
<0.001 |
|
Renal |
12 (3.4) |
5 (2.6) |
7 (4.3) |
0.365 |
|
Neurosurgical |
50 (14.0) |
29 (14.9) |
21 (12.9) |
0.589 |
|
Respiratory |
15 (4.2) |
9 (4.6) |
6 (3.7) |
0.660 |
|
Gynecologic |
2 (0.6) |
0 |
2 (1.2) |
0.121 |
|
Othersb
|
16 (4.5) |
7 (3.6) |
9 (5.5) |
0.378 |
Table 2.Outcomes and resource use according to period
|
Characteristics |
All patients |
2007–2012 |
2013–2017 |
P-value |
|
Support during index ICU stay |
|
|
|
|
|
Mechanical ventilation |
432 (33.9) |
205 (34.7) |
227 (33.2) |
0.585 |
|
Ventilator weaning (n=432) |
273 (63.2) |
120 (58.5) |
153 (67.4) |
0.056 |
|
Noninvasive ventilation |
15 (1.2) |
4 (0.7) |
11 (1.6) |
0.123 |
|
Vasopressor |
414 (32.5) |
174 (29.4) |
240 (35.1) |
0.030 |
|
Renal replacement therapy |
99 (7.8) |
50 (8.5) |
49 (7.2) |
0.393 |
|
CAG |
59 (4.6) |
32 (5.4) |
27 (4.0) |
0.216 |
|
Outcome |
|
|
|
|
|
ICU mortalitya
|
163 (12.8) |
86 (14.6) |
77 (11.3) |
0.076 |
|
28-day ICU mortality |
145 (11.4) |
77 (13.0) |
68 (10.0) |
0.071 |
|
In-hospital mortalitya
|
228 (17.9) |
126 (21.3) |
102 (14.9) |
0.001 |
|
ICU LOS |
3.0 (1.0–6.0) |
3.0 (1.0–7.0) |
2.0 (1.0–6.0) |
0.283 |
|
Hospital LOS |
12.0 (6.0–24.0) |
13.0 (6.0–28.0) |
11.0 (5.0–22.0) |
0.041 |
Table 3.Univariate and multivariate Cox regression analysis addressing the risk factors for intensive care unit in-hospital mortality
|
Variable |
Univariate analysis
|
Multivariate analysis
|
|
OR |
95% CI |
P-value |
OR |
95% CI |
P-value |
|
Age |
1.036 |
0.993–1.082 |
0.104 |
|
|
|
|
Men |
1.022 |
0.784–1.333 |
0.871 |
|
|
|
|
SOFA score |
1.049 |
1.020–1.078 |
0.001 |
0.979 |
0.946–1.013 |
0.218 |
|
ICU admission due to medical reason |
2.034 |
1.454–2.845 |
<0.001 |
0.990 |
0.615–1.594 |
0.969 |
|
Admission source |
|
|
|
|
|
|
|
Ward |
Reference |
|
|
|
|
|
|
Emergency room |
1.819 |
1.289–2.567 |
0.001 |
1.970 |
1.247–3.112 |
0.004 |
|
Others |
1.534 |
0.605–3.894 |
0.368 |
2.220 |
0.837–5.883 |
0.109 |
|
Underlying disease |
|
|
|
|
|
|
|
Hypertension |
0.974 |
0.734–1.292 |
0.855 |
|
|
|
|
Chronic heart disease |
0.770 |
0.558–1.064 |
0.114 |
|
|
|
|
Solid tumor |
0.560 |
0.264–1.190 |
0.132 |
|
|
|
|
DM |
1.087 |
0.820–1.441 |
0.562 |
|
|
|
|
Chronic kidney disease |
1.047 |
0.554–1.978 |
0.888 |
|
|
|
|
Cerebrovascular accident |
1.378 |
0.956–1.986 |
0.085 |
|
|
|
|
Laboratory findings |
|
|
|
|
|
|
|
White blood cell (×103/ul) |
1.032 |
1.022–1.042 |
<0.001 |
1.005 |
0.984–1.025 |
0.663 |
|
Platelet (×103/ul) |
0.999 |
0.997–1.000 |
0.092 |
0.999 |
0.997–1.001 |
0.601 |
|
Albumin (g/dl) |
0.720 |
0.583–0.891 |
0.002 |
0.871 |
0.660–1.150 |
0.331 |
|
T-bilirubin (mg/dl) |
1.115 |
1.041–1.193 |
0.002 |
1.060 |
0.961–1.168 |
0.244 |
|
Creatinine (mg/dl) |
1.266 |
1.181–1.357 |
<0.001 |
1.234 |
1.085–1.402 |
0.001 |
|
C-reactive protein (ng/ml) |
1.021 |
1.007–1.035 |
0.004 |
0.992 |
0.972–1.013 |
0.438 |
|
Support during index ICU stay |
|
|
|
|
|
|
|
Ventilator weaning |
0.062 |
0.037–0.104 |
<0.001 |
0.064 |
0.036–0.115 |
<0.001 |
|
Vasopressor |
2.954 |
2.246–3.884 |
<0.001 |
1.550 |
1.004–2.394 |
0.048 |
|
Renal replacement therapy |
3.434 |
2.555–4.614 |
<0.001 |
1.035 |
0.658–1.629 |
0.882 |
|
2013–2017 (compared to 2007–2012) |
0.803 |
0.618–1.044 |
0.101 |
|
|
|
References
- 1. KOSIS. 100 Indicators of KOSIS [Internet]. Daejeon, KOSIS. 2021;[cited 2021 May 17]. Available from: https://kosis.kr/visual/nsportalStats/index.do?menuId=all.
- 2. Kim KW, Kim OS. Super aging in South Korea unstoppable but mitigatable: a sub-national scale population projection for best policy planning. Spat Demogr 2020;8:155-73.ArticlePubMedPMCPDF
- 3. Al-Dorzi HM, Tamim HM, Mundekkadan S, Sohail MR, Arabi YM. Characteristics, management and outcomes of critically ill patients who are 80 years and older: a retrospective comparative cohort study. BMC Anesthesiol 2014;14:126. ArticlePubMedPMCPDF
- 4. Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, et al. The APACHE III prognostic system: risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991;100:1619-36.ArticlePubMed
- 5. Lim JU, Lee J, Ha JH, Kang HH, Lee SH, Moon HS. Demographic changes in intensive care units in Korea over the last decade and outcomes of elderly patients: a single-center retrospective study. Korean J Crit Care Med 2017;32:164-73.ArticlePubMedPMCPDF
- 6. Williams TA, Dobb GJ, Finn JC, Webb SA. Long-term survival from intensive care: a review. Intensive Care Med 2005;31:1306-15.ArticlePubMedPDF
- 7. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993;270:2957-63.ArticlePubMed
- 8. Lee SH, Lee TW, Ju S, Yoo JW, Lee SJ, Cho YJ, et al. Outcomes of very elderly (≥ 80 years) critical-ill patients in a medical intensive care unit of a tertiary hospital in Korea. Korean J Intern Med 2017;32:675-81.ArticlePubMedPMCPDF
- 9. Giannasi SE, Venuti MS, Midley AD, Roux N, Kecskes C, San Román E. Mortality risk factors in elderly patients in intensive care without limitation of therapeutic effort. Med Intensiva (Engl Ed) 2018;42:482-9.ArticlePubMed
- 10. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996;22:707-10.ArticlePubMedPDF
- 11. Nguyen YL, Angus DC, Boumendil A, Guidet B. The challenge of admitting the very elderly to intensive care. Ann Intensive Care 2011;1:29. ArticlePubMedPMCPDF
- 12. Garland A, Olafson K, Ramsey CD, Yogendran M, Fransoo R. Epidemiology of critically ill patients in intensive care units: a population-based observational study. Crit Care 2013;17:R212. ArticlePubMedPMC
- 13. Moran JL, Bristow P, Solomon PJ, George C, Hart GK, Australian and New Zealand Intensive Care Society Database Management Committee (ADMC). Mortality and length-of-stay outcomes, 1993-2003, in the binational Australian and New Zealand intensive care adult patient database. Crit Care Med 2008;36:46-61.ArticlePubMed
- 14. Sim YS, Jung H, Shin TR, Kim DG, Park SM. Mortality and outcomes in very elderly patients 90 years of age or older admitted to the ICU. Respir Care 2015;60:347-55.ArticlePubMed
- 15. Kwak SH, Jeong CW, Lee SH, Lee HJ, Koh Y. Current status of intensive care units registered as critical care subspecialty training hospitals in Korea. J Korean Med Sci 2014;29:431-7.ArticlePubMedPMCPDF
- 16. Kim J, Lee J, Choi S, Lee J, Park YS, Lee CH, et al. Trends in the use of intensive care by very elderly patients and their clinical course in a single tertiary hospital in Korea. Korean J Crit Care Med 2016;31:25-33.ArticlePDF
- 17. Kim DY, Lee MH, Lee SY, Yang BR, Kim HA. Survival rates following medical intensive care unit admission from 2003 to 2013: an observational study based on a representative population-based sample cohort of Korean patients. Medicine (Baltimore) 2019;98:e17090.PubMedPMC
- 18. Lee SH, Hong JH, Kim YS, Park EC, Lee SM, Han CH. Impact of intensivist and nursing staff on critically ill patient mortality: a retrospective analysis of the Korean NHIS cohort data, 2011-2015. Yonsei Med J 2021;62:50-8.ArticlePubMedPDF
- 19. Kim S, Kim TH. The association between nurse staffing level and length of stay in general ward and intensive care unit in Korea. Appl Nurs Res 2022;63:151558. ArticlePubMed
- 20. Oh TK, Song IA. Trends in mortality, treatment, and costs of management of acute respiratory distress syndrome in South Korea: analysis of data between 2010 and 2019. Yonsei Med J 2022;63:452-60.ArticlePubMedPMCPDF
- 21. Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA 2014;311:1308-16.ArticlePubMed
- 22. Roch A, Wiramus S, Pauly V, Forel JM, Guervilly C, Gainnier M, et al. Long-term outcome in medical patients aged 80 or over following admission to an intensive care unit. Crit Care 2011;15:R36. ArticlePubMedPMC
- 23. Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med 1998;26:1793-800.PubMed
- 24. Salluh JI, Soares M. ICU severity of illness scores: APACHE, SAPS and MPM. Curr Opin Crit Care 2014;20:557-65.PubMed
- 25. Htwe TH, Mushtaq A, Robinson SB, Rosher RB, Khardori N. Infection in the elderly. Infect Dis Clin North Am 2007;21:711-43.ArticlePubMed
- 26. Martin-Loeches I, Guia MC, Vallecoccia MS, Suarez D, Ibarz M, Irazabal M, et al. Risk factors for mortality in elderly and very elderly critically ill patients with sepsis: a prospective, observational, multicenter cohort study. Ann Intensive Care 2019;9:26. ArticlePubMedPMCPDF
- 27. Mukhopadhyay A, Tai BC, See KC, Ng WY, Lim TK, Onsiong S, et al. Risk factors for hospital and long-term mortality of critically ill elderly patients admitted to an intensive care unit. Biomed Res Int 2014;2014:960575. ArticlePubMedPMCPDF
- 28. Atramont A, Lindecker-Cournil V, Rudant J, Tajahmady A, Drewniak N, Fouard A, et al. Association of age with short-term and long-term mortality among patients discharged from intensive care units in France. JAMA Netw Open 2019;2:e193215.ArticlePubMedPMC
- 29. Vallet H, Schwarz GL, Flaatten H, de Lange DW, Guidet B, Dechartres A. Mortality of older patients admitted to an ICU: a systematic review. Crit Care Med 2021;49:324-34.ArticlePubMed
- 30. de Rooij SE, Abu-Hanna A, Levi M, de Jonge E. Factors that predict outcome of intensive care treatment in very elderly patients: a review. Crit Care 2005;9:R307-14.ArticlePubMedPMC
Citations
Citations to this article as recorded by

- Chronicles of change for the future: The imperative of continued data collection in French ICUs
Takashi Tagami
Anaesthesia Critical Care & Pain Medicine.2023; 42(5): 101294. CrossRef - We need a comprehensive intensive care unit management strategy for older patients
Dong-Ick Shin
Acute and Critical Care.2022; 37(3): 468. CrossRef
 , Younsuck Koh2
, Younsuck Koh2 , Jin Won Huh2
, Jin Won Huh2 , Sang-Bum Hong2
, Sang-Bum Hong2 , Chae-Man Lim2
, Chae-Man Lim2





 KSCCM
KSCCM
 PubReader
PubReader ePub Link
ePub Link Cite
Cite